Health crisis in the bush leaves Australians without GPs as News Corp pushes for more support during the election
Australia’s rural health is at a new crisis point. Hundreds of rural towns don’t have a doctor, there is a six week wait to see one and pregnant women are even being handed DIY birth kits. It’s time to act.
Illness
Don't miss out on the headlines from Illness. Followed categories will be added to My News.
Exclusive: More than 850 rural towns are advertising for a doctor, there is a six week wait to see a country GP and pregnant women are being handed DIY birth kits as rural obstetric units close.
Five years after News Corp Australia won major increases in subsidies of up to $60,000 to attract more doctors to small rural towns, the health crisis in the bush has intensified.
PM tight-lipped on election date
Mystery of who invited ‘Human Ken doll’ to Budget solved
People in the bush are dying on average two years earlier than people in the city, they have three times the rate of chronic illness, more mental health problems and the suicide rate in remote communities is two and a half times that in cities.
Yet country people see doctors at only half the rate of people in metropolitan areas and they see specialists at one third the rate, according to Royal Flying Doctor Service CEO Mr Martin Laverty.
Mums are facing a four-hour trips to give birth, with more than four in ten maternity units around Australia having closed in recent years, most of them in small country towns.
This has led to a 47 per cent increase in babies born before mothers can reach a hospital, a recent study found.
The lack of maternity services is killing babies.
In towns without a maternity unit 23.3 babies in 1000 are dying compared with 6.1 per 1000 in rural towns with services.
Many country towns can’t attract even a single GP let alone the psychologists, physiotherapists and dentists they need and the problem is so bad people in the bush want it to be a major election issue.

“This election cannot be allowed to pass without both sides of politics spending more and ensuring doctors and health professionals get to the areas where they are needed,” Dr Laverty said.
The number of doctors graduating from university has more than doubled in the last decade and subsidies have been increased to attract graduates to the bush but young doctors won’t move there in the numbers needed.
Graduates who do move to the bush don’t always want to work in the local hospital, work full time or provide after-hours care and aren’t trained in obstetrics or anaesthetics.
Doctors groups are calling for radical new solutions. Today News Corp begins a campaign for:
• Federal government funding for fly in fly out GPs in towns that can’t attract a doctor;
• $72 million a year in federal funding for 500 fly in fly out allied health workers like dentists; physiotherapists and mental health workers for the bush;
• Federal funding for salaried GPs in small towns where Medicare funding is too small to make a living;
• Expanded Medicare funding for telehealth to cover GP consultations in the bush at a cost of $180m a year;
• Salaries for trainee country GPs, as well as maternity leave, plus credit towards long service leave;
• The implementation all recommendations of the 2018 Senate inquiry into accessibility and quality of mental health services in rural and remote Australia;
• Reform of the GP rural incentive payment to reward doctors who provide greater scope of service such as advanced and after hours treatment; and
• A rural loading for specialists to incentivise them to provide services in the bush.
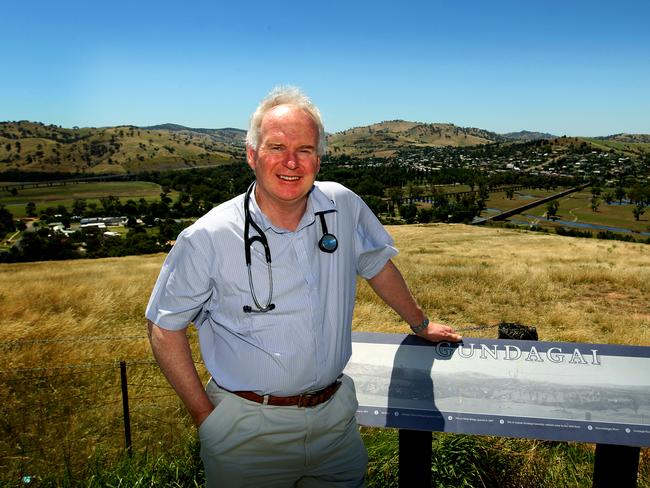
“It’s time for taxpayers to ask why are we spending all this money increasing the number of people going through training to end up in the oversupplied cities when we can’t get doctors into our country towns.” said former president of the Rural Doctors Association and Gundagai GP Dr Paul Mara.
He said the Federal Government should licence practices and restrict new practices to areas where they are needed.
The Rural Doctors Association argues a key part of the problem is that we don’t have a comprehensive training program for bush doctors that attracts rural students and equips them with the skills they need to be a country doctor including obstetrics and anaesthetics.
NSW and Queensland are trialling new training programs where trainee rural doctors work under an industrial award with safe working hours, maternity leave and long service leave.
The doctors are offered a training program with mentoring and support, plus options to get skills in obstetrics and anaesthetics.
This week’s federal budget provided $62 million for the national roll out of this kind of rural generalist training pathway but it will be a decade before that pushes graduates out the other end.

That’s why the Royal Flying Doctor Service’s Dr Laverty believes we need a stopgap measure to improve services now by providing fly-in fly-out doctors and allied health workers.
Rural health experts support this idea but said for it to work it must provide continuity of care, the same doctors and health providers must return regularly to the communities they service rather than pay for a different provider each visit.
Another key part of the solution is Medicare funding for telephone consultations by rural GPs and salaries or some kind of block funding for those in small towns.
Dr Laverty said “Medicare is not working for all Australians” and doctors can’t make enough income from it in towns with less than 2,000 people so we need to consider paying salaries or block funding doctors in small towns.
THE GREAT QUACK QUEST OF TEMORA
When the NSW town of Temora learned it was losing it longest serving GP late last year it knew it had to stand out from the other 850 rural towns desperately searching for a doctor.
Showing their imagination and good humour, the townspeople donned dancing shoes and produced a quirky YouTube video called The Great Quack Quest.
“We wanted to showcase the community, to show that this is a good place to come and that you’ve got to be right for the community if you want to be our doctor,” said local GP Dr Rachel Christmas, the brains behind the video.
“Being in the country can be good and a doctor can add great value to a community,” said Dr Christmas who started out as an engineer before retraining as a GP and returning to her home town where she now works part-time as a GP obstetrician.
The nature of rural practice is changing and country towns need even more doctors than ever, she said.
“The traditional male doctor whose wife was a nurse, that’s changed and doctors don’t work long hours and there are more women doing general practice and they don’t want to work full-time hours,” she said.
Although the town of 4000 currently has nine doctors only three are permanent full-time and they are all due to retire in the next five years.
“People may think it’s cheeky of us using the term ‘quack’ but we have a sense of humour. We can’t keep doing what everyone else is doing,” said Temora’s Mayor Rick Firman.
Twelve years ago when the town needed a doctor the town offered a $500,000 incentive, Dr Rodney Kurtzner answered the call but he didn’t want the money.
He’s still practising today.

Dr Christmas said getting more rural kids into medical school and rolling out a rural generalist pathway is critical to reducing the shortage of doctors in the bush.
Mr Firman said Temora was a great place to live with five schools, 45 sporting clubs, a picture theatre, a heated pool, a sporting complex for rugby league, Aussie rules, cricket, soccer, rugby squash and tennis and a trotting track.
Temora is also home to the famous harness racer Paleface Adios who won 109 races from 204 starts in the 1970s.
The Town’s quirky job advertisement has already attracted a few responses.
LIFE SAVING RESCUE
Belinda Bennett had worrying symptoms for 12 months but difficulty accessing a doctor in her tiny town meant her bowel cancer diagnosis was delayed and her cancer progressed.
Three hours drive from doctors in Broken Hill, the Bennett family live on a remote sheep station in the centre of Australia and are on the frontline of Australia’s rural doctor crisis.
The nearest town of Tilpa only gets a visit from a fly in fly out doctor once a month and the town of Wilcannia, 80 kilometres away, only has a fly in fly out doctor three days a week.
Poor access to medical care meant Belinda’s bowels had stopped working before she finally sought help when the Royal Flying Doctor Service made their regular monthly visit in 2011.
She then faced a three-hour drive to Broken Hill to get a colonoscopy.
She recalled that after the procedure the doctor said “‘I am really sorry to tell you that you have a tumour so big, it’s blocking your bowel. We need to get you to Adelaide before you burst’.”

The cancer returned in 2013 and again she had to drive to hundreds of kilometres to Broken Hill and then Adelaide for treatment.
“I drove three hours one way to Broken Hill every month for chemotherapy and every second week drove to Wilcannia to have my line flushed,” she said.
“Then there was a tough six weeks of radiotherapy when I was by myself in Adelaide without family, it was stressful for me,” says Mrs Bennett.
Two of the family’s three children broke bones when they fell off their motorbikes and had to be evacuated by the Royal Flying Doctor Service.
And when her husband Todd broke two vertebrae, Mrs Bennett had to drive him at slow speed to the nearest bitumen airstrip to be evacuated by the Royal Flying Doctor Service in a neck brace.
“We need more medical specialists coming out to see remote people more often,” the 49-year-old mother and grandmother.
Mrs Bennett would especially like a dermatologist to visit to check her extended family for skin cancer.
“It’s really tricky because you do need to go further afield for major issues,” she said.

Originally published as Health crisis in the bush leaves Australians without GPs as News Corp pushes for more support during the election


