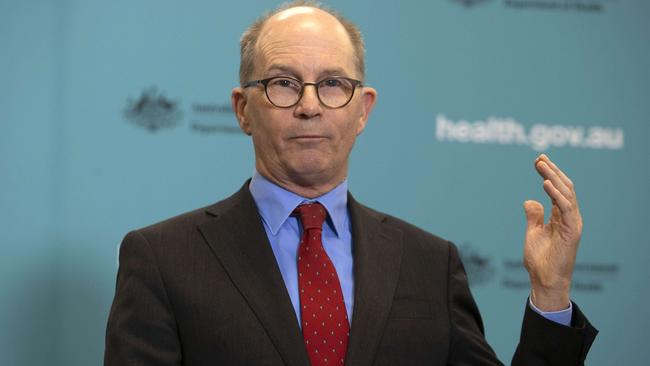
Chief Medical Officer Paul Kelly backs AstraZeneca COVID-19 vaccine to save lives in Australia
Australia’s chief medical officer has hosed down criticism of the Melbourne-made COVID-19 vaccine, declaring it will work.
Coronavirus
Don't miss out on the headlines from Coronavirus. Followed categories will be added to My News.
Australia’s top doctor has slapped down medicos criticising our coronavirus vaccination plan and assured Australians the jabs they receive will save lives and prevent severe illness.
Chief Medical Officer Professor Paul Kelly accused some doctors of stoking “controversy” about the Melbourne-made AstraZeneca jab, declaring it would be “very effective” in stopping the worst symptoms of COVID-19.
The Pfizer vaccine, developed with new mRNA technology, rated as more effective than the AstraZeneca option in clinical trials, although both were successful in preventing serious health problems and keeping coronavirus patients out of hospital.
Nobel Prize-winning immunologist Professor Peter Doherty told the Herald Sun the AstraZeneca vaccine would provide critical protection for Australians, as Prof Kelly warned focusing on “selective” data was undermining public confidence.
“The choice is not whether one is better than the other, it’s which one is available to give the maximum rollout of vaccine to save lives and to protect lives this year,” Prof Kelly said.
“The answer to that is the one we can make here.”
The Pfizer drug is expected to be the first cleared for use this month. It will be shipped in and given to five million Australians most in need including aged care residents and staff, frontline healthcare workers, and border and quarantine officials.
The Herald Sun understands the federal government is considering building a domestic mRNA manufacturing facility, but it would take at least a year to develop, while it is also in negotiations with other vaccine providers.
The Pfizer jab rated as at least 90 per cent effective in trials, compared to 62-90 per cent for AstraZeneca in its trial which reported in early December.

Prof Kelly said both — if approved by the Therapeutic Goods Administration — would prevent serious symptoms and exceed the World Health Organisation’s goal of 50 per cent effectiveness.
Prof Doherty said: “60 per cent (effectiveness) for someone like me has worked on influenza is a pretty good vaccine.”
“We’ve got a world where a lot of people are dying and a lot of others will suffer long-term debilitating effects,” the Doherty Institute patron said.
“With the vaccines we’ve got … it does provide a measure of protection.”
While there is little research on whether coronavirus vaccines successfully reduce transmission and create herd immunity, that will be reviewed as doses are delivered.
Australian and New Zealand Immunology Society president Professor Stephen Turner was reported as saying on Tuesday he would not widely roll out AstraZeneca “because of that lower efficacy”.
But the society later shot that down, saying it was a “robust and safe vaccine” and an “important advance” in tackling the pandemic.
Federal medical chiefs will now brief outspoken experts who have criticised the vaccination program, in an effort to reduce misinformation.
Prof Kelly warned public confidence was at risk, with government research finding about one in five Australians were already wary of receiving the vaccine.
“Some people have been taking particular parts of that (AstraZeneca research) article and not reading the whole article,” Prof Kelly said.
“Confidence is absolutely the most important thing, and that’s what worries me about the coverage we had.”

Prof Doherty said while there was “a lot of unknowns”, a less effective vaccine — if proven safe — was better than nothing, and he was willing to roll up his sleeve for a jab.
“We’ve never tried to vaccinate our way out of a rapidly spreading pandemic before,” he said.
“It’s really a whole new ballgame. I don’t think any product will go to waste.”
CSL is making 50 million doses of AstraZeneca in Melbourne, enough for the whole population, which Prof Kelly said saved Australia from competing with other countries.
The federal government has also purchased 51 million doses of Novavax, which is yet to finish clinical trials.
Another agreement with the global COVAX facility secured access to extra vaccines for half the population, potentially providing more Pfizer doses and Moderna’s mRNA jab, although these would take longer to deliver.
Opposition health spokesman Chris Bowen said the government should have locked in agreements for more vaccine candidates.
But Professor Allen Cheng, co-chair of the government’s immunisation advisory panel, said: “If you were in charge of a vaccine manufacturer, would you send your supply to a country where there are thousands of deaths a day or to Australia?”




