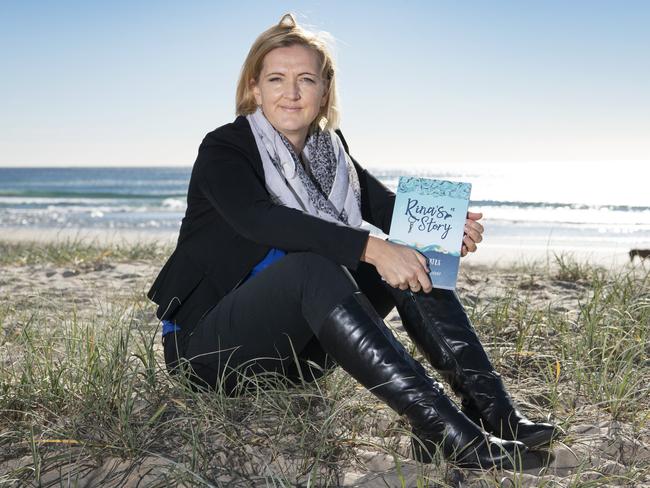
Dr Tash Yates’s warning: ‘Don’t become a GP, we’re broken’
This beloved Gold Coast GP’s confession rocked the city’s medical fraternity, and should strike fear in the heart of every resident and potential patient. Here’s what she had to say.
Gold Coast
Don't miss out on the headlines from Gold Coast. Followed categories will be added to My News.
Dr Tash Yates could not believe what she had just done.
After more than 20 years practicing as one of the Gold Coast’s most beloved GPs, it felt wrong … but she knew it was right.
And so the Mudgeeraba General Practice doctor took to Twitter to confess:
“I just counselled a junior doctor NOT to train as a GP,” she tweeted.
“Cannot believe it has come to this!
“I’ve spent two decades practicing and advocating for my speciality, but this young woman has her future ahead of her, and I’d hate to see her undervalued, unsupported and burnt out.”
It’s an admission that rocked the city and country’s medical fraternity, and one that should strike fear in the heart of every resident and potential patient.
Because without our GPs … well, we’re stuffed.
Already the symptoms of this broken system can be seen across the Coast, with doctors abandoning general practice or slashing their hours, with private practices crying out for more physicians, with patients left infuriated as they are unable to make a timely appointment, with the number of junior doctors training in the once-competitive field of general practice dwindling to critical levels.
And as for Bulk Billing? Be careful what you wish for … being left out of pocket might be the least of your worries.
The facts and figures of our GP crisis speak for themselves:
The Medicare rebate for a short consultation has barely budged in 10 years, rising just over $4 in a decade - from $35.60 to $39.75.
Meanwhile, the AMA-recommended fee for a standard consultation is around $86.
This may be a problem involving doctors, but you don’t need to be a brain surgeon to recognise that inflation and cost-of-living pressures have taken their toll when it comes to delivering healthcare, yet those same economic influences have somehow left the rebate untouched.
In fact, when it comes to the grand total that Australia spends on healthcare, about 90 per cent goes to hospitals, and only 6.5 per cent to primary healthcare such as general practice.
This despite the fact that, according to the Australian Bureau of Statistics, almost 84 per cent of Australians saw a GP in 2021-22, compared to 14 per cent presenting to an emergency department, and 12 per cent admitted to hospital.
While the Federal Government recently released the Strengthening Medicare Taskforce Report, which aims to reform the ageing system, it did not mention any increase to Medicare rebates.
Instead, there has been a narrative unravelling that our GP crisis comes down to doctors asking for more money.
For Dr Yates, that is what truly sickens her. She says the truth is that GPs are only advocating for more cash in the pocket of the patient.
“The Medicare rebate is not something that goes to doctors … it goes to patients. That’s why we want more - we want patients to get more money back so that healthcare is more equitable.
“A general practice is a small business. Just like when you pay for a meal at a restaurant, the wait staff does not pocket that money, it goes to the business.
“The fee for a standard consultation is not just for the doctor’s time and expertise, it covers our administration staff, our nurses, our IT, the premises, all of our consumables.
“To think that can all be covered in less than $40 is unconscionable. Yet that is what doctors who bulk bill are trying to do … and that’s the part that really makes me worry.
“What are they cutting back on to make that happen? I truly hope it’s not something that will compromise patient care.
“Quite often it’s the wages of the doctor, because GPs are altruistic … but that’s hardly healthy, not for the doctor, not for the practice and not for the future of the speciality.”
And that leads to precisely why Dr Yates sent that tweet: her industry is on the brink of complete burnout.

She says most GPs work as contractors, meaning they do not receive sick leave, maternity leave or holiday pay and are only paid a percentage for the patients they see.
They also self-fund their insurance and continued professional development, which can run into the tens of thousands each year.
Meanwhile, for every hour Dr Yates works, there’s another 30 minutes of unpaid paperwork. For every patient she sees with a complex issue, particularly mental health, the clock is ticking … and the caseload just keeps piling up.
And for every hope for future change, she sees no meaningful action in the present.
“Sending that tweet was a reaction to what was probably one of my lowest moments,” she says.
“That was a student of mine I’ve known for years, she’s now a junior doctor. I’d been a referee for her and she was always so excited to get on the GP program.
“Now she’s been offered other options within the hospital system and was talking it through with me. She’s looking at a mortgage and starting a family and I just couldn’t advise her in good faith to pursue being a GP.
“The uncertainty right now is just too high. Don’t get me wrong, hospitals have their own issues, but at least she feels supported there and is working as part of a team.
“I could only tell her what I would tell my own daughter.
“For 14 years we’ve been calling out about this crisis with Medicare - the rebate has not kept up with the cost of living, we have an ageing population which means even more pressure on the system and I just can’t see any real change that indicates a better system is in the wings.
“I truly believe we will look back in 10 years and see 2023 as the year that makes or breaks our system. This year will decide whether, when we are old, we will be able to access quality health care quickly and equitably.
“It seems dramatic, but I’m just reading the room.
“Being a GP is not a job for me, not even a career … it’s a calling. But it’s at the point where I have to step back and look at the harm it’s doing.”
While Dr Yates says it hurts to see her colleagues suffer, her greatest concern goes to the patients.
She says the Gold Coast was historically a city with a surplus of GPs, due to its lifestyle advantages, but it’s now facing the same practice shortages as the rest of the country, with an even higher demand due to our older demographic.
She says while Medicare has become a political football, constantly kicked but never scoring points, the city and country need a bipartisan approach to cure the system.
“We’re already seeing residents unable to book a doctor and unable to afford a doctor … people are hurting,” she says.
“Then we’re hearing this line about ‘greedy doctors’ … it couldn’t be further from the truth. We are doing the best we can to see everyone and charge the least we can without going broke - and losing an entire practice.
“There are already gaps showing up on the Coast, patients are waiting weeks to get an appointment. Practices are closing and doctors are slashing hours … you might have the same number of doctors, but half the number of hours.
“I see colleagues posting on social media, they’re now in education, or writing, or podcasting … they need a break before they’re broken.
“The biggest problem is that governments are blaming the GPs. That’s why we’re trying to convey the truth - this is a problem not of our making and therefore we can’t solve it. This is something that needs to be solved at a political level, but without becoming a political issue.
“We are sick of being the scapegoat.
“The fact is that because funding for primary health care comes from the federal government, while state government funds hospitals, the federal government doesn’t really care if someone is not getting excellent preventative health care because when they have to go to hospital - well, that’s a state government problem.
“That federal government inaction is not party specific, this has been a problem growing over more than a decade, with both sides overseeing it.
“It’s like divorced parents fighting, but it’s the children - in this case, the patients - who suffer.
“This problem is solvable, but it’s going to take political will that breaches not only the party divide but the federal and state divide.
“If doctors are suffering, the community is suffering. GPs are not the problem but the symptom. It’s time to start complaining about the real problem to the right people.”
Perhaps it’s time for politicians to take an oath:
First, do no harm.





