‘Silent killer’: Covid infection may cause an inflammatory response in the brain
Researchers at an Australian university have discovered a previously unknown effect Covid appears to have on the human brain.
Science
Don't miss out on the headlines from Science. Followed categories will be added to My News.
Researchers at an Australian university have found that Covid-19 activates the same inflammatory response in the brain as Parkinson’s disease, potentially putting people at greater risk of developing neurodegenerative conditions.
A team at the University of Queensland’s School of Biomedical Sciences, led by Professor Trent Woodruff and Dr Eduardo Albornoz Balmaceda, joined with virologists from the School of Chemistry and Molecular Biosciences for the study, whose findings have been published in the scientific journal Molecular Psychiatry.
“We studied the effect of the virus on the brain’s immune cells, ‘microglia’, which are the key cells involved in the progression of brain diseases like Parkinson’s and Alzheimer’s,” said Prof Woodruff.
“Our team grew human microglia in the laboratory and infected the cells with SARS-CoV-2, the virus that causes Covid-19. We found the cells effectively became ‘angry’, activating the same pathway that Parkinson’s and Alzheimer’s proteins can activate.”
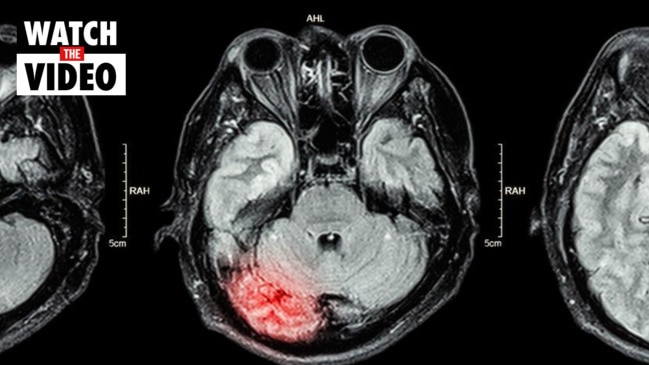
Activating that pathway creates a “fire” in the brain, which leads to a “chronic and sustained” process of killing off neurons.
“It’s kind of a silent killer, because you don’t see any outward symptoms for many years,” Dr Albornoz Balmaceda explained.
“It may explain why some people who’ve had Covid-19 are more vulnerable to developing neurological symptoms similar to Parkinson’s disease.”
Want to stream your news? Flash lets you stream 25+ news channels in 1 place. New to Flash? Try 1 month free. Offer available for a limited time only >
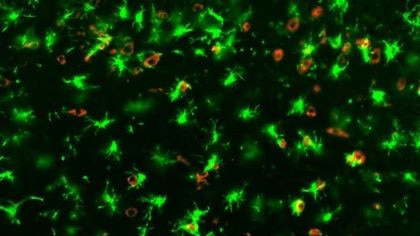
The researchers found the effects of a Covid infection were exacerbated if there were already proteins in the brain linked to Parkinson’s.
“If someone is already predisposed to Parkinson’s, having Covid could be like pouring more fuel on that ‘fire’ in the brain,” Prof Woodruff said.
“The same would apply for a predisposition for Alzheimer’s and other dementias that have been linked to inflammasomes.”
The study did include a hint of better news however, with the researchers identifying a potential treatment for the inflammation.
Administering inhibitory drugs developed by the University of Queensland, which are currently being used in clinical trials with Parkinson’s patients, “successfully blocked the inflammatory pathway activated by Covid”.
In other words, the drugs were “essentially putting out the fire”, Dr Albornoz Balmaceda said.
“The drug reduced inflammation in both Covid-infected mice and the microglia cells from humans, suggesting a possible treatment approach to prevent neurodegeneration in the future,” he said.
“Further research is needed, but this is potentially a new approach to treating a virus that could otherwise have untold long-term health ramifications,” added Prof Woodruff.
New Covid variant reaches Australia
This comes as Australia wrestles with the arrival of a new, vaccine-resistant variant of Covid known as XBB, which recently shot up from causing a fifth of Australia’s infections to more than half of them in just a week.
The XBB strain, which is believed to be more resistant to both vaccines and antibodies from previous infections, emerged in Singapore weeks ago and is now spreading here.
“It is likely the most immune-evasive and poses problems for current monoclonal antibody-based treatments and prevention strategy,” Amesh Adalja, a public health expert at the Johns Hopkins Centre for Health Security, told The Daily Beast.
There is no need to panic, however. People who are fully vaccinated are far less likely to become seriously ill if they contract the new strain, and Pfizer and Moderna’s new “bivalent” vaccines are effective at fighting it off.
Australia recorded about 30,000 new Covid cases last week, and infections have been increasing gradually.
Professor Peter Collignon, an infectious diseases expert, said there was no evidence the new XBB strain was “more virulent, as judged by hospitalisations and deaths”.
And Professor Catherine Bennett, an expert from Deakin University, said hybrid immunity in Australia would now be a lot higher than it was when the Omicron strain arrived last year.
“More than half the population has been both vaccinated and had an infection, and that does put you in a more resilient position when facing future waves,” Prof Bennett said.
“We won’t see the same high hospitalisation and high death numbers that we saw between December and July, because that’s when all the variants were circulating and people were basically getting infected for the first time.”
Originally published as ‘Silent killer’: Covid infection may cause an inflammatory response in the brain



