Ricky ‘Dougie’ Hampson death: Family walked out of court during inquest when doctor apologises
The grieving family of an Aboriginal man who was misdiagnosed at a regional hospital and died less than 24-hours after being discharged has walked out of court during the doctor’s formal apology. Here’s the latest.

Dubbo News
Don't miss out on the headlines from Dubbo News. Followed categories will be added to My News.
The doctor who misdiagnosed an Indigenous man with a cannabis-related condition, before he died less than 24 hours after being discharged from a regional hospital, formally apologised to his family as they walked out of the courtroom.
Aboriginal and Torres Strait Islander readers are advised this article contains the name and images of a person who has died.
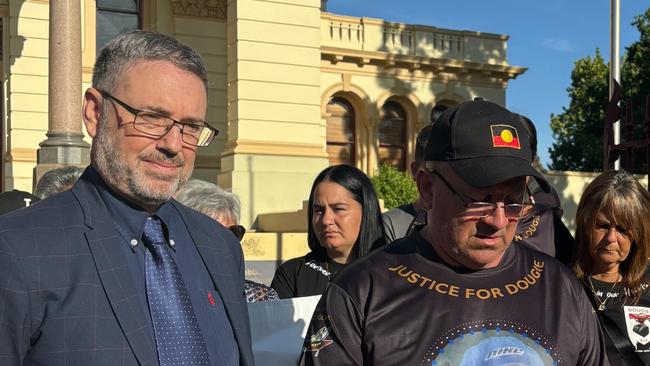
The probe into the death of 36-year-old Kamilaroi-Dunghutti man Ricky “Dougie” Hampson Junior on August 16, 2021, has heard a doctor, apologise to Mr Hampson’s family after he gave evidence at the coronial inquest in Dubbo.
“I’m very sorry for your loss – I wish I could go back and change things … this will sit with me for the rest of my life,” he said.
Mr Hampson’s family walked out of the courtroom as the apology was delivered.
Mr Hampson went to Dubbo Base Hospital on August 14, 2021, experiencing severe stomach pain and a “popping” and “tearing” sensation in his abdomen.

He was diagnosed with cannabinoid hyperemesis syndrome (CHS) – a condition relating to long-term marijuana use – by a doctor after he was given pain-relief and sedative medication by a junior doctor.
Despite not experiencing nausea or vomiting, which are common symptoms of the diagnosis, he was given sedative medication to alleviate the pain.
Mr Hampson was also given IV fluid to manage his dehydration and initial bloods were taken.
No further investigations were conducted to confirm the diagnosis, including an X-ray or a CT scan, and he was discharged the following day.
An autopsy revealed he died at a friend’s house less than 24-hours after being discharged from the hospital because of two perforated ulcers.
The doctor told the court he was first made aware of Mr Hampson when his junior doctor asked for advice of the situation.

He said she told him the patient had abdominal pain, was agitated but does not recall a “popping” sound being discussed.
The doctor told the court he did not recall Mr Hampson mentioning the sound either.
He said since the incident and internal investigation, the hospital had made significant changes to ensure another misdiagnosis is not delivered.
He told the court he had a “conscious bias” when diagnosing patients with CHS as it mainly affected Indigenous patients.
“I’ve changed my practice when I see patients of Indigenous background,” he said.
He said he had made an effort to respect customs, beliefs and outcomes when coming to a diagnostic approach.
He admitted there was not an issue with ordering imaging on the night.
He also said he should have asked the junior doctor when Mr Hampson began experiencing the pain and how it started.



