Royal Hospital for Women forced to ‘borrow’ mammogram machine
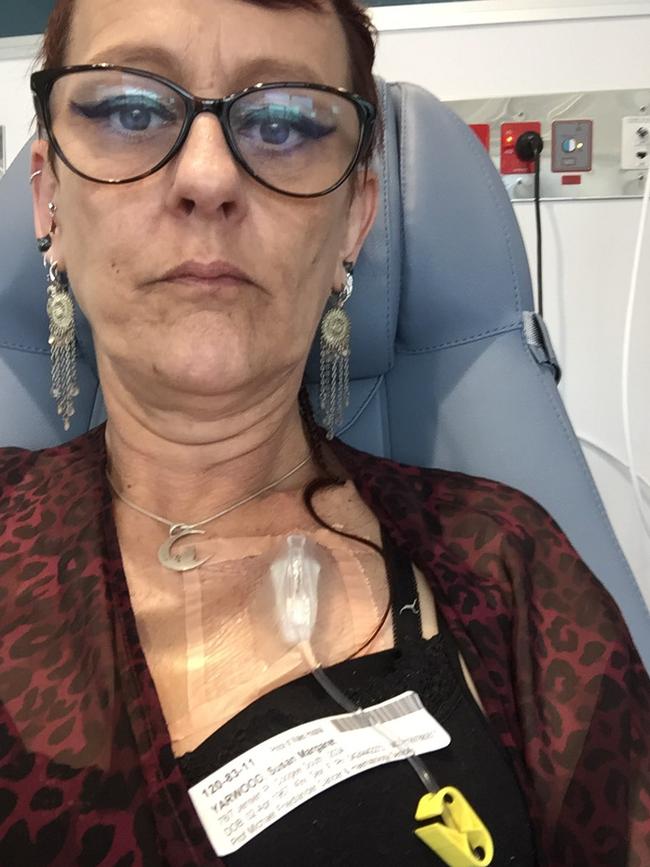
It is the premier women’s hospital in the state, yet the Royal Hospital for Women does not have it’s own mammogram machine, instead it is forced to borrow one, leaving women waiting too long for a diagnosis. Breast cancer survivors Monique Correy and Sue Yarwood are supporting a fundraiser for a new machine.
NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
The only hospital in the state dedicated to women’s health does not have a mammogram machine.
The Breast Centre at the Royal Hospital for Women has to borrow one from BreastScreen NSW but can only use it three days a week.
The centre sees more than 2500 patients a year from all over the state.
RHW Director of Breast Care services Dr Alex Matthews said it was “bizarre” the hospital did not have its own machine to diagnose breast cancer.
“The RHW runs a diagnostic service for people that have a symptom which could be cancer and gets investigated by mammography, ultrasound and clinical examination — but we don’t have our own mammography machine,” Dr Matthews told The Sunday Telegraph.

BreastScreen NSW offers free screening mammograms to women aged 50-74. A screening mammogram is a test for well women, designed to pick up breast cancers before they can be felt or seen.
A diagnostic mammogram, which is a test for women who have symptoms like a lump — which could indicate breast cancer — is what the RHW desperately needs.
The share arrangement of the mammogram machine with the BreastScreen NSW, which shares the same space in the hospital, is leading to unacceptable waitlists doctors say.
“If you have cancer it is important to be seen promptly. Most people say a standard of care is to have a diagnosis within days and once diagnosed to have treatment within a fortnight,” Dr Matthews said.
“People are just beside themselves if they have lump because they are worried it could be malignant.
“I think it is pretty poor. We need the ability to diagnose and manage breast disease promptly and that means state-of-the-art equipment, no borrowed machinery.”

Breast cancer is the most common cancer diagnosed in Australian women. It has a 91 per cent survival rate — of at least five years — due to early diagnosis.
It accounts for about 29 per cent of all new cancers in Australian women and one in seven will develop breast cancer in their lifetime.
Kirsten Pilatti, CEO of Breast Cancer Network Australia said the situation was “crazy” but not isolated to RHW.
Neither Campbelltown nor Liverpool Hospitals have their own mammography machines for diagnosis either.
“We need to look at the investment around diagnostic because it is a time women are anxious about, any time period they have to wait is unacceptable,” she said.

Sarah McGill, Director of Cancer Screening and Prevention, Cancer Institute NSW, oversees the BreastScreen NSW program, said a number of BreastScreen services in NSW have share agreements in place within their local health district.
But the shared equipment also means there is no free follow-up on offer for those who need annual screening post a cancer diagnosis Ms Pilatti said.
“We have issues in Campbelltown where there are no public options to access mammograms or ultrasounds for follow-up,” Ms Pilatti said.
Once diagnosed with breast cancer, patients are required to have annual check-up mammograms due to the higher risk of the cancer returning.
“For follow-up care, post diagnosis, what is happening in that situation is women that can’t afford it, which in Campbelltown would be many, they simply don’t have their follow up mammograms.
“Clinicians are saying to me patients are not doing it or being forced to pay up to $500 to go privately to have their follow-up care, which is out of reach for many.”
* Next Friday night, the Foundation will host The Harper’s Bazaar In Bloom dinner at The Art Gallery of NSW. Donate at royalwomen.org.au/bazaar
BREAST CANCER SURVIVORS
By the time Bondi Public School teacher Christie Fyson discovered she had breast cancer in 2017, it was already stage three.
The 41-year-old was dismayed when she learned the RHW Breast Centre did not have its own mammogram machine.
“Once I’d got the results from my ultrasound saying I needed to come back, they said I had to wait three weeks because there was such a backlog of patients queuing for that shared machine,” she said.
“I just couldn’t wait three weeks, I knew it was bad and I could feel the lymph gland.
“My GP managed to take matters into her own hands and got me into see the surgeon a lot faster so I didn’t have to wait.”

Coogee mother of two and now grandmother Sue Yarwood was diagnosed with breast cancer in 2016 but had to use a private service for her mammogram at a cost of $200. It found a 7.5cm lump.
“You just assume the mammogram used at the Royal is theirs but to only have it three out of five days is ridiculous,” the 52-year-old said.
“The better the mammogram, the better the diagnosis and the better access the less you have to wait.”

When Monique Correy felt a lump when she was getting dressed last October, she too went to a private clinic where she was also diagnosed by biopsy and ultrasound.
“I was told there were long wait lists to get a mammogram and I didn’t have that time to wait, so it wasn’t an option, I had to go back to the private clinic,” the 27-year-old from Double Bay said.
Ms Correy had a double mastectomy and six months of chemotherapy. She said the RHW needs its own mammogram.
“I think for all women, it’s so important to have early detection. This machine will help thousands of women detect cancer early which is lifesaving,” Ms Correy said.


Now the RHW is trying to raise $750,000 to buy and run its own machine.
Trish O’Brien, chief executive of The Royal Hospital for Women Foundation, said not having their own machine was impacting on delivering a world-class service to women.
“Evidence clearly shows that the early detection of breast cancer with high quality equipment is a crucial element in saving lives, yet our capacity is being limited by the lack of equipment,” she said.
