NSW nurses say they are struggling in emergency department ‘war zones’
Nurses in hospitals across NSW say they are working double shifts, skipping meal breaks and returning to work less than eight hours after finishing their prior shift – yet there still isn’t enough staff to keep on top of their patient loads.
NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
Sick and vulnerable patients are falling through the cracks, forced to wait hours for treatment in emergency departments that can resemble a “war zone” according to struggling frontline workers.
Nurses in hospitals across NSW say they are working double shifts, skipping meal breaks and returning to work less than eight hours after finishing their prior shift – yet there still isn’t enough staff to keep on top of their patient loads.
Kelly Falconer has been a nurse in The Central Coast region for 26 years and said the pressure on nurses had “never been so bad”, with her emergency department often resembling a “war zone”.
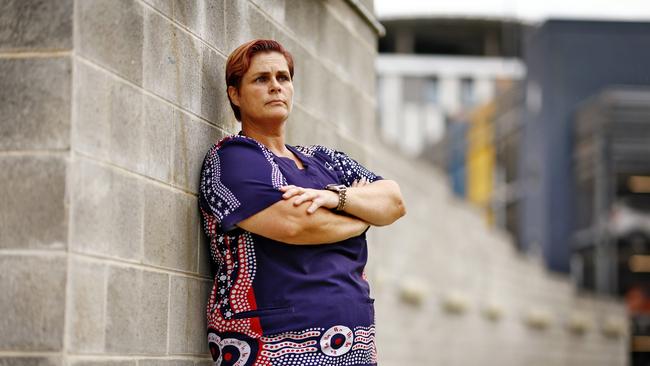
“We are really struggling at the moment, the exhaustion and the struggle is very real. We’ve got senior nurses who just don’t want to do this anymore,” Ms Falconer, the NSW Nurses and Midwives Association Wyong branch president, said.
“Our workload is constantly increasing yet our resources are decreasing.”
In a letter obtained by the Saturday Telegraph, a nurse from Coffs Harbour Base Hospital wrote to the heads of the hospital saying nurses were so stretched that patients in the emergency department were facing a real risk of “serious adverse outcomes”.
The nurse, who remained anonymous in the letter, said the hospital was often on bed block, which meant it was common to see more than 30 inpatients in the emergency department waiting for a bed.
“Many of these patients spend more than 24 hours in ED and around 10 per cent of these patients never make it to a ward, spending their entire hospital stay in ED,” the nurse wrote.
“An important consequence of access block is that new patients who require access to monitored beds (eg palpitations, chest pain abdominal pain) are often unable to access
appropriate (monitored) beds and are frequently being managed in areas of ED which are inappropriate, unmonitored and unsafe.”

In response to questions about the letter, a NSW Government spokesperson said staffing at the hospital had increased by 25 per cent over the past five years.
“Attracting and retaining healthcare staff in rural and regional areas is a longstanding, fundamental challenge faced by all state and territory health systems across Australia,” they said.
“Coffs Harbour Health Campus has welcomed several intakes of new nursing and midwifery graduates this year. The District is recruiting more than 150 international nurses, more than half of whom will be working at Coffs Harbour Health Campus with 17 already joining the ranks.”
The hours have become so bad for some nurses across the state – they are leaving the industry altogether, while others are facing burnout, extreme stress and job dissatisfaction according to NSW Nurses and Midwives Association general secretary Shaye Candish.
“There is a lot of anxiety (for our nurses) because they know that they’re walking into a shift that’s going to be short staffed and how difficult that’s going to be even before they get there,” she said.
“A lot of them feel pressured to pick up extra shifts because they’ll see lots of text messages come out asking for someone to work overtime, and someone always feels compelled to go in or work the double shift.
“And that’s how our hospitals are functioning.”
Ms Candish said that by 2025, the nation was predicted to have a shocking nursing shortfall of 85,000 staff – which would only worsen the wait times for patients, and create immense strain on nursing staff.
“The workload is already so heavy that many nurses have decided they don’t want to do it anymore,” she said.
“(They are) required to be available seven days a week, they work night shifts, work weekends, and that’s a lot of sacrifice in terms of work life balance.

“So we need to do a lot more not just to keep people in the job, but attract more to it.”
The NSW Government recently announced that from the beginning of this month, hundreds of additional nurses and midwives will be recruited at the state’s busiest EDs to improve safe-staffing levels.
Liverpool Hospital and Royal North Shore are the first of the level five and six ED’s receiving extra nursing staff, which the government expects to reach safe staffing levels by July.
The government spokesperson said the nursing retention rate in NSW had increased to above 93 per cent in 2024, with more than 3400 new graduate nurses and midwives recruited for employment so far this year.
“Local health districts and specialty health networks also continue their recruitment efforts with a range of social media and advertising campaigns in Australia and abroad,” they said.
“The NSW Government is delivering on its promise to roll out safe staffing levels in NSW public hospitals, meaning more nurses and midwives between now and July 2027.”
Got a news tip? Email weekendtele@news.com.au





