Heart monitor health insurance claims rejected for cardiac patients
Insurers are being accused of turning a blind eye to vulnerable cardiac patients – leaving them to foot the bills for remote heart monitors despite signing an agreement to cover the costs.
NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
- Heartbroken family: ‘Pray for the driver who killed our daughter’
- What you get as a Daily Telegraph subscriber
Health insurers are being accused of fobbing off cardiac patients, leaving them to foot the bill for crucial remote monitors, despite earlier agreeing to cover costs for critical cases.
High clinical need patients with pacemakers and defibrillators who applied to get a remote heart monitor are being rejected by Medibank, AHM and nib, cardiologists claim.
Peak body Private Healthcare Australia signed an agreement with the Cardiac Society of Australia and New Zealand on September 2, seen by The Daily Telegraph, reiterating they will cover the cost of the device – an average $1450 – on an ex-gratia basis.
The monitors are on the Federal Government’s Prostheses List and have been reimbursed by funds when provided as part of a hospital procedure since 2015.
But the CSANZ estimated there are about 2000 Australians with high clinical need who do not have the device, either because it wasn’t provided with their surgery or because procedure happened before 2015.
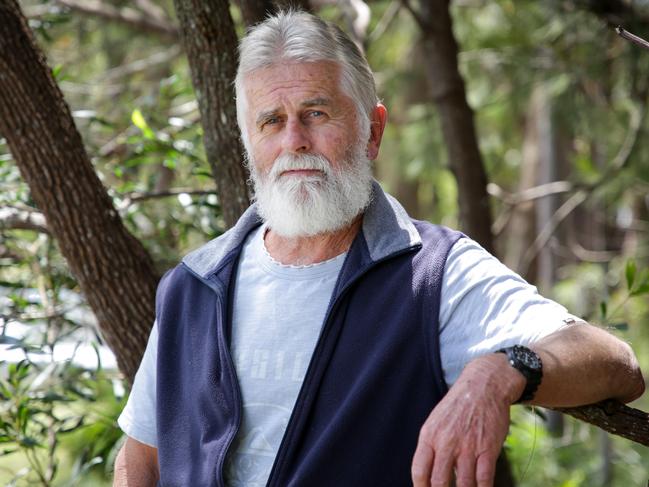
Newcastle pensioner John Mullington had two applications rejected by AHM.
“It has been very frustrating. (My doctor) said I need more regular monitoring and getting to see him can be a lengthy process which is why he suggested the monitor,” the 68-year-old said.
“$1450 is very expensive. It is very hard to exist on a pension.”

CSANZ Heart Rhythm Council Chair Professor Saurabh Kumar said insurers were contradicting government advice to reduce traffic to hospitals during COVID-19.
“(Insurers) all agreed it’s a good idea and it was a great victory. (Now) they need to do what they have promised to do.”
Cardiologist Dr Bradley Wilsmore said none of his submissions since the agreement have been approved yet.
“It is on all the guidelines. The standard of care is to have a monitor. It’s frustrating.”
The Daily Telegraph has seen rejection letters from Medibank, nib and AHM and many did not provide a reason.
PHA boss Rachel David said the government was cost shifting.

“Health inflation is rising, the cost of the device is rising not just faster than any other country but this is also the only area pushing premium up,” she said.
“We can’t afford to have a single extra cost on the system.”
Ms David said it was unclear why patients who previously have not needed a heart monitor needed one now.
Hearts4Heart charity head Tanya Hall said clinicians would not file an application without a genuine need.
“These are all high clinical need patients, this is why the clinicians are heavily advocating it, it’s an insult to clinicians.” she said.

Medibank and AHM medical chief Dr Linda Swan said they will treat the applications “seriously”.
“(If a) cardiologist tells us their patient has an urgent clinical need for remote monitoring, our Clinical Team will take the advice of the treating specialist seriously,” she said.
A nib spokesman responded: “Nib actively encourages alternative health and treatment pathways, particularly if they avoid unnecessary hospitalisation for our members. We’re supportive of recent changes to pay a benefit (for remote monitors).”
A Federal Health spokesman said the government expects insurers and healthcare providers to work together on the issue.
“It is important to note the private health insurance regulatory framework provides significant flexibility for private health insurers and healthcare providers to enter into contractual arrangements for the provision of care, whether in hospital or out of hospital,” he said.
“The Government expects the insurers and healthcare providers to work together to make use of this flexibility so that patients have access to high quality, cost effective services that meet their needs and make private health insurance an attractive product.”

