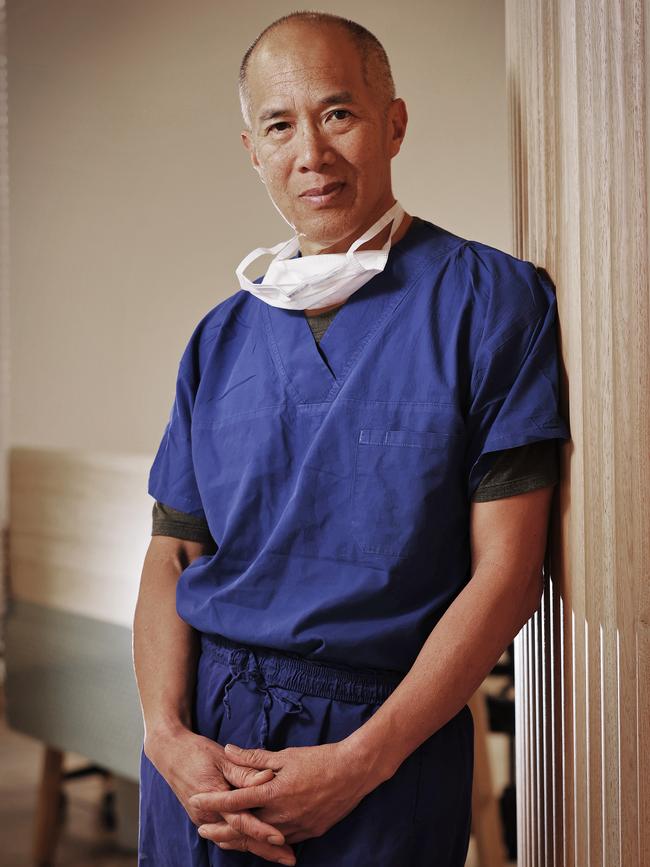
Desperate parents heap praise on ‘lifesaving’ neurosurgeon Charlie Teo
Madeline Suy was diagnosed with the deadliest of brain tumours that no surgeon wants to touch. Then her father met Dr Charlie Teo.

NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
Madeline Suy was diagnosed with the deadliest “worst of the worst” brain stem tumour that no surgeon wants to touch, let alone remove, and kills children within a year of diagnosis.
The diffuse intrinsic pontine glioma (DIPG) is one of two forms of tumour considered “inoperable” that has landed Dr Charlie Teo in hot water with the NSW Medical Council.
Madeline’s dad, Alan, knew of the controversy surrounding Dr Teo’s radical approach to such tumours, but says that “as a parent of a young child who has been given a death sentence, where survival is measured in months, you desperately search for hope and options”.
“I appreciate that one of the reasons why Dr Teo is being restricted in Australia is because he provides a contrary opinion to patients with DIPG. However, there is no other neurosurgeon in Australia who has done as many surgeries on the brain stem than he has,” Mr Suy said.
“The extensive surgical experience that Dr Teo has accumulated over his 30-plus-year career, which has been published in multiple peer-reviewed journals legitimises his contrary opinion – a course of action which may provide outcomes that some parents may not be ready for mentally, but which other parents like me and my wife were more than willing to accept.”

Mr Suy is one of dozens of parents who have reached out to share their experience of dealing with a potentially fatal brain cancer diagnosis.
He said he “wants to make it very clear that Dr Teo never offered any kind of false hope”.
“He was very honest and forthright in his pre-operative consent, and told us in no uncertain terms that his approach was unconventional, high-risk and came with no guarantees of success,” he said.
“One could argue the fact that Dr Teo is offering a contrasting opinion on how to handle DIPG, whereas other doctors are not offering any contrasting opinions or even another approach, is the very reason why he should be allowed to practise unrestricted in Australia.”
The controversy surrounding Dr Charlie Teo’s decision to operate on brain stem tumours, particularly DIPG, has prompted dozens of former and current patients to come forward.
Dr Teo told The Saturday Telegraph this week the debate around “inoperable” brain stem tumours was a complicated one and misinformation was rife, even among neurosurgeons in Australia and around the world.
Virtually every intrinsic primary brain stem tumour is labelled as DIPG because there is “no real definition and no one wants to talk or think about having to operate on them”, he said.
“That’s why all these authorities are saying Teo is operating when he shouldn’t.
“No, they have got it all wrong.”
It was the brave and innovative US-based paediatric neurosurgeon Fred Epstein who was credited for pioneering neurosurgical techniques to treat children with brain stem and spinal cord tumours.
He was the first to recognise there were two very distinct brain stem gliomas — focal and diffuse, Dr Teo said.
“Unfortunately, his progressive approach to these tumours didn’t really catch on and hence, until this day, no one has clearly identified radiological or clinical criteria to differentiate one from the other,” he said.
“Everyone has their own definition of what is diffuse. That’s why there is this often tragic confusion throughout the entire paediatric neuro-oncology world.”
Dr Teo has developed a method for differentiating focal gliomas from diffuse gliomas, based on the high volume of brain stem tumours he has seen over the last 30 years.
“I get hundreds of cases of these types of tumours sent to me from across the globe and with that sort of experience I have developed my own criteria that helps me differentiate,” he said.
“Once I’ve decided it is focal or that it has a focal component then I consider it to be operable. If it’s purely diffuse then there’s no way I’m going to touch it.”
Dr Teo said in the last five years he has come across only four tumours that fit into a third category – a diffuse tumour with a focal component.
“I’m not here boasting about my amazing results but I believe when you have a diffuse tumour with a focal component you can give a patient some benefit by operating,” he said.
“Out of the four that I have done, three had very good outcomes. One case had a tragic outcome. That was soul-destroying as the patient never woke up after surgery, a terrible result for both the patient and the family.

“Once you start exploring and looking for advancements, you are going to get some bad outcomes, some terrible outcomes, which I have had.
“You are also going to have patients that do very well, that get more months or years on their lives and get to enjoy life.
“One man in Germany was days away from dying when I operated on him in Stuttgart three years ago and he is still alive today and enjoying life.”
Madeline’s parents consider she is one of the good three outcomes and, although they don’t know what the future holds, they know they have bought their little girl more time.
“Dr Teo had clearly explained to my wife and I that the tumour was of a diffuse nature, but there were also some focal parts which he believed was safe to take out,” Mr Suy said.
“The diffuse part of the tumour could not be taken out as it was too risky, and if he had made the mistake of taking the diffuse part of the tumour out, it would badly injure her and potentially paralyse her.
“My research prior to meeting Dr Teo made me aware of the risk of serious injury that could occur for such high-risk surgery in the brain stem. It is one of the sensitive surgeries which has caused much controversy for Dr Teo.
“He made us aware of the risks, such as dying on the operating table. It was an extremely tough decision to make and one that needed much consideration.”
Madeline had a six-hour surgery at Prince of Wales Private Hospital on December 15, 2020. Post-op MRI scans showed “a significant debulking of the tumour”.
Another MRI scan taken after six weeks of radiation therapy saw a further shrinkage of the tumour in the brain stem region.
In mid-June 2022, nearly 18 months after Madeline’s surgery, MRI scans confirmed that the tumour was again growing.
This week, two months after her eighth birthday which her parents didn’t think she would reach, Madeline remains asymptomatic.

“Statistically speaking, Madeline has already beaten the odds, as the average survival time for DIPG patients is nine to 12 months,” Mr Suy said.
“While the tumour is in progression, It is at a slower rate than originally anticipated.”
When Dr Teo again saw MRI scans in August this year, he advised the family that surgery “was not an option at this stage”.
The family is looking at other options, including clinical trials, to extend Madeleine’s life for as long as possible with the hope that a cure is around the corner.
She is currently enrolled in the PINOC-022 trial to test promising new drug combinations.
“My wife and I are extremely grateful to have had Dr. Charlie Teo’s guidance and support. His surgery eradicated her migraines, restored her co-ordination and extended her survival,” Mr Suy said.
“Dr Teo had discussed all the risks of performing the surgery. He had repeatedly told us that Madeline could end up in a wheelchair paralysed if he made a mistake during the procedure.
“Looking back, my wife and I are still unanimous that we made the right decision.”
OUR SON IS ALIVE: THAT’S WORTH PRICE
Harry Cross was happily playing in the park when his mother noticed the three-year-old’s eyes suddenly turn inward.
An MRI revealed the worst possible news. Harry had a tumour on his brain stem, a focal low grade brain stem glioma.
Doctors at the Sydney Children’s Hospital told Lynda and Doug there was not much they could do – the tumour was inoperable because of its location.
But one neurosurgeon suggested Charlie Teo might be the only one who could help, Mr Cross explained.
“Long story short, Charlie was brought in, we listened to what he had to say, then he did the first operation and got 90 per cent,” Mr Cross said.
“It started coming back so he had to do another op just under a year later and a third one close to two years later.”
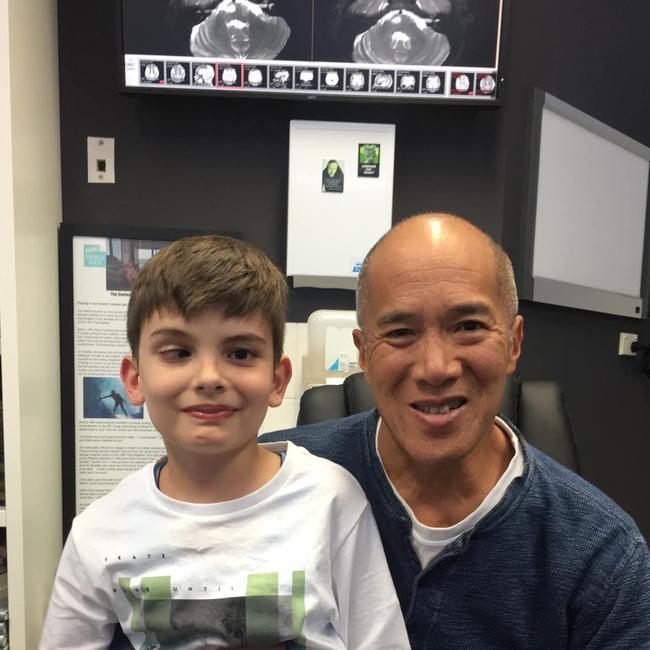
Harry is now 12 and “touch wood” his scans are showing no signs of any new tumour.
“There’s nothing there now. The hole is closing over. A few months ago when we saw Charlie he said we don’t have to come any more,” Mr Cross said.
“If it wasn’t for Charlie, Harry wouldn’t be here now because no one else wanted to do it.”
Brainstem tumours account for 10 to 20 per cent of all childhood brain cancers.
The radical surgical resection of focal brain stem gliomas can be performed “with acceptable risk in well-selected cases and likely confers survival advantage for what is otherwise a rapidly and universally fatal disease” according to the World Neurosurgery journal 2021.
Mr and Mrs Cross said they are saddened that Dr Teo is no longer operating in Australia and shudder to think what that would mean should Harry need more surgery.
“It’s true that I am no longer able to operate in Australia, not because I’ve lost my licence, but because the Prince of Wales Private Hospital would not renew my privileges, claiming that my surgeries were too high risk.” Dr Teo said.
“And subsequent applications to other hospitals that perform neurosurgery are denied once the doctors at those hospitals are consulted.”
The Cross family scoffed at suggestions Dr Teo prayed on vulnerable families and over- charged.
“He told us all the risks, he told us what could go wrong, and he told us all the costs,” Mr Cross said.
“None of the surgeries were over $100,000, and in fact one of them was covered by our health fund. But what would you do in this situation? Not operate?
“We saw the itemised bill of how that money was shared among the hospital, the other doctors, that’s what happens in these high-risk surgeries.”
Dr Teo told The Saturday Telegraph this week his charging practices as a neurosurgeon are in line with those of other professionals in the field.
“As you can appreciate, not all brain surgeries are equal, and the amount charged is based on a range of factors. While some surgeries are relatively quick and safe, other can take hours or involve particularly difficult work,” he said.
“It is generally accepted practice for a surgeon not to charge the same fees for a simple 45-minute surgery as for a complicated 18-hour tumour resection.
“The bulk of the costs are the hospital fees, with the remainder of the costs being split between a variety of health professionals including the surgeon, anaesthetist, pathologist, radiologist and intensivist.”
Using one example of a complex case, the total cost of the medical procedure was about $120,000, and in that situation about $80,000 goes to the private hospital for its fees, while the remaining $40,000 is shared between the various health professionals, Dr Teo said.
Some patients, particularly those without private health insurance, choose to crowdfund to help cover the costs.
Dr Teo said he still has had a longstanding policy over the last 20 years of offering to operate on any patient in the public system, in their hometown and under Medicare — essentially at zero cost to the patient.
This can be done if a patient’s local neurosurgeon invites Dr Teo to their hospital.
Dr Teo operated twice at the Children’s Hospital Westmead pro bono in recent years.
Cydonee Mardon is a former patient of Dr Teo



