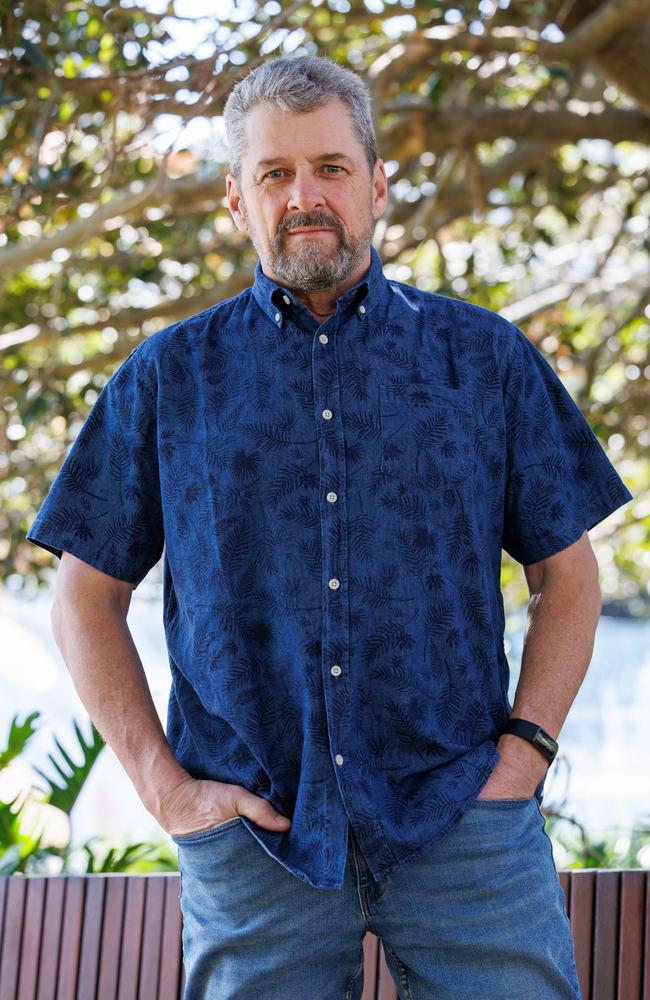
Dan Colgan will use voluntary assisted dying after battle with brain cancer
Dan Colgan has been diagnosed with an incredibly rare and aggressive brain cancer. Instead of pursuing treatment, he has decided to end his own life.

NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
Dan Colgan will end his own life. Since making the decision, he has never felt more alive.
The 63-year-old Western Australian resident has an incredibly rare and aggressive brain cancer. There is no cure. No hope of recovery.
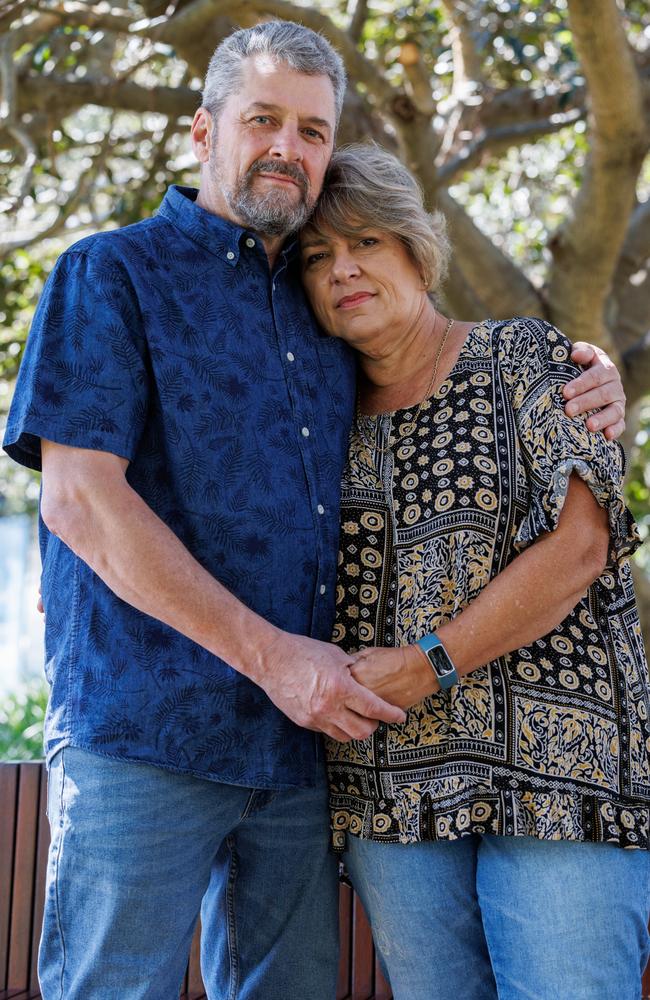
Instead of going through rounds of chemotherapy, the adoring husband of Laury, and father of four and granddad of two decided to withdraw treatment altogether and access Western Australia’s legalised voluntary assisted dying program.
“Since we’ve made that decision, suddenly everything else fell into focus. We completely stopped thinking about dying. Now that the dying has been taken care of, I can just focus on the living,” he said.
In less than two months, on November 28, voluntary assisted dying will be legal in NSW, allowing terminally ill residents to end their life, just as Dan will.

In the 18 months since the Voluntary Assisted Dying Act was passed in May 2022, NSW Health has thrown itself into preparation. With military-like precision implementation teams have worked together to plan exactly how the VAD will work.
On Friday, more than 700 nurses, GPS, pharmacists, aged care workers, and members of the public gathered in person and online at the NSW Voluntary Assisted Dying Conference in Sydney.
NSW chief health officer, Dr Kerry Chant, who heads up the rollout, said that while it is a little scary to think that the process will be available in a little over eight weeks, “we are absolutely committed to being ready.”
Clinical Lead of the implementation team, Dr Wade Steadman, said the NSW team followed in the footsteps of other states.
“I’m very happy that we are going last. We’ve had great support from our colleagues from interstate we’ve learned a lot from them and as a result we will have a really great system for patients.”
“We are on track to deliver a safe and effective service accessible to eligible people who wish to access voluntary assisted dying across the state, with particular planning underway to support people in regional remote areas,” he said.
Unlike other states like Victoria, in NSW, nurses, doctors and other health practitioners will be allowed to initiate discussions about VAD to terminal patients.
To be eligible, people must be over the age of 18, a NSW resident for 12 months, have a decision-making capacity throughout the entire process, and make a first request to doctors that is “clear and unambiguous.”
“Anyone who permanently loses decision making capacity in relation to voluntary assisted dying will no longer be eligible,” said Dr Chant.

Patients need to be access voluntarily without pressure and duress. They must have a terminal illness that is advanced, progressive and will cause death within six months, or in the case of neurodegenerative within 12 months.
The condition must be causing people suffering in a way that cannot be relieved in a way that is considered tolerable.
To apply for VAD access, patients must go through an 11 step process, involving independently and specially trained practitioners, a number of formal, written requests, and formal assessments and reviews conducted by a newly constructed Voluntary Assisted Dying Board.
“A healthcare worker is not obligated to participate in voluntary assisted dying process,” said Dr Chant.
Once a patient receives final approval from the board, they will have two options for ending their life; self-administration or practitioner administration.
Those who choose to end their lives themselves can do so in two forms; by drinking an “incredibly bitter” liquid, the patient will prepare themselves, or via an enthral feeding device.
Those choose to use practitioner administration can have it intravenously.
According to Professor Michael Dooley, Director of Victoria’s Voluntary Assisted Dying Pharmacy Service, most patients choose oral medication.
“It‘s the most bitter thing you’ve tasted. I’ve tasted it. It’s horrible. They have to swallow 30ms. It is not easy.”
The drugs work extremely quickly and painlessly. According to Professor Dooley, once taken, the medications always work.
“Patients fall asleep within one or two minutes. It‘s really quick. We tell patients once you start do not stop. Don’t stop halfway through and say how terrible it tastes because you might fall asleep before you finish it.”
“A large proportion of patients will [die] in under 30 minutes. We do have patients that last longer that go longer than 2 hours. We have had some go for 12 hours.”
For Dan Colgan, method is irrelevant. What matters most, is that people have choice.
“What you’re gaining is choice and self-determination. Nothing is being taken away. There is no downside to this.
“I could have spent the remaining months of my life in fear and concern for myself and my family, wondering what the end would be like. Now I know all that. There is no fear anymore,” he said.





