Game-changing blood test for breast cancer could dramatically improve survival rates
Too often when breast cancer returns it is picked up too late but a new blood test could help find it earlier and dramatically improve survival rates.
National
Don't miss out on the headlines from National. Followed categories will be added to My News.
A game-changing blood test that could detect when breast cancer returns could save lives and mean women can get treated quickly before the disease spreads further.
Garvan Institute researcher Professor Clare Stirzaker has identified 30 DNA biomarkers in the blood linked to breast cancer and is working to turn the knowledge into a blood test that can be run overnight.
In less than 10 years – and for less than $100 – she hopes women who have a history of breast cancer can take regular blood tests to check whether their cancer has returned and have it picked up earlier than through current methods.

While most patients respond well to initial treatment, the disease returns in about 16 per cent of women, and there are currently no reliable or sensitive tests to identify these relapses early.
The research is one of 20 projects to share in $12.4 million in National Breast Cancer Foundation (NBCF) funding.
Professor Stirzaker will use the funding to develop a smaller panel of DNA markers for breast cancer and reduce the time it takes to do the test from around a week to less than 24 hours.
“It’s much easier way to monitor people rather than having to do a tumour biopsy, for instance, which is much more invasive,” she said.
The test is not yet sensitive enough to detect early stage breast cancer which does not shed enough DNA so mammograms will still be needed, she said.
“I DID NOT EXPECT A RECURRENCE”
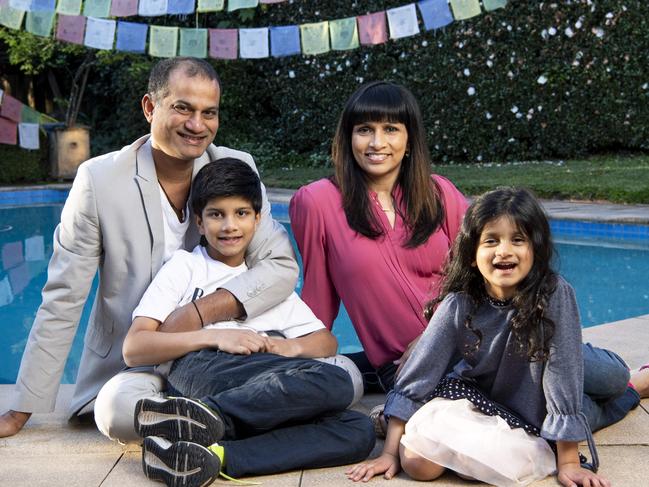
For Jo Fernandes a blood test that could tell her breast cancer had returned might have saved her from four gruelling months of chemotherapy.
The 47-year-old psychologist first developed breast cancer in 2014 when her son was 18 months old and she was just 39.
“The first thing I thought was what many people think ‘Will I die from this?’,” she said.
When her doctor began talking about what treatments she would need “all I could see was my little baby boy on the floor playing with his Matchbox cars was while I’m being told I’ve got cancer,” she said.
She had surgery and radiotherapy and “life was sweet again” especially after she gave birth to a miracle baby girl at age 42.
But in 2017 her cancer returned.
“That hit me for six. I did not expect a recurrence,” she said.
Friends and family rallied around to help her as she struggled through chemotherapy while trying to care for her young baby and son.
“Now that research is looking into a blood test to detect cancer early, I think wow that could be a huge game changer for some people – it’s amazing to think that perhaps a blood test could detect recurrence,” she said.
“This research has the potential to stop invasive treatments like chemotherapy and major surgery that many people have to endure currently. Hopefully with the idea that a blood test could detect a tumour earlier than what they do now could be less invasive and a huge benefit to a cancer patient – the earlier the cancer is found the better.”
Ms Fernandes said she wanted to tell her story to give people hope.
“It’s not always a death sentence which so many women still think, but treatments and preventative measures are improving and there is so much research being done,” she said.
“A lot of women get quite depressed and anxious after a diagnosis, it takes quite a mental toll. I want to provide hope, that I came out of it twice and finding it early gave me a much better chance of surviving cancer.”
GOAL TO ELIMINATE DEATHS FROM THE CANCER BY 2030
National Breast Cancer Foundation CEO Associate Professor Cleola Anderiesz said the five year survival rates for breast cancer “are much higher if you detect the cancer early and you treat it early”.
“Five year survival rates for stage one breast cancer are actually around 100 per cent but the moment we get to metastatic cancers, they become much harder to treat. And the survival rate plummets significantly for these to around 32 per cent,” she said.
“So the ability to pick up that recurrence of cancer early (using a blood test) offers that opportunity to provide the earlier therapeutic intervention and hopefully increase their chance of survival,” she said.
Monash University’s Professor Tony Tigani has received NBCF funding to investigate how obesity influences the development of triple negative breast cancer and its response to immunotherapy and examine ways to enhance the response of therapies in all patients.

Professor Georgia Chenevix-Trench from QIMR-Berghofer has funding to repurposing Senicapoc, a drug originally developed for the treatment of sickle cell anaemia, to treat a group of triple negative breast cancers with poor prognosis.
The NBCF has invested nearly $200 million into almost 600 research projects since 1994 to help increase the five-year survival rate for breast cancer from 76 per cent to 91.5 per cent.
“This equates to nearly 50,000 women and men who have survived to their five-year milestone thanks to funding from the generous Australian community and shows that leading-edge research is the key to stopping deaths from breast cancer,” Professor Cleola Anderiesz said.
The foundation has a goal of eliminating deaths from the cancer by 2030.



