Terrifying reason for groom’s ‘stress headache’
Simon Goodrich was on his honeymoon when a crippling “stress headache” left him fighting for his life.
Illness
Don't miss out on the headlines from Illness. Followed categories will be added to My News.
At 26, Simon Goodrich was recently married and celebrating his honeymoon, when life threw a golf ball-sized curve ball at him.
“I’d had a whole series of headaches that year,” explains the 43-year-old Melbourne man, “I’d put them down to stress, but then we went away on our honeymoon, and the symptoms just got worse.”
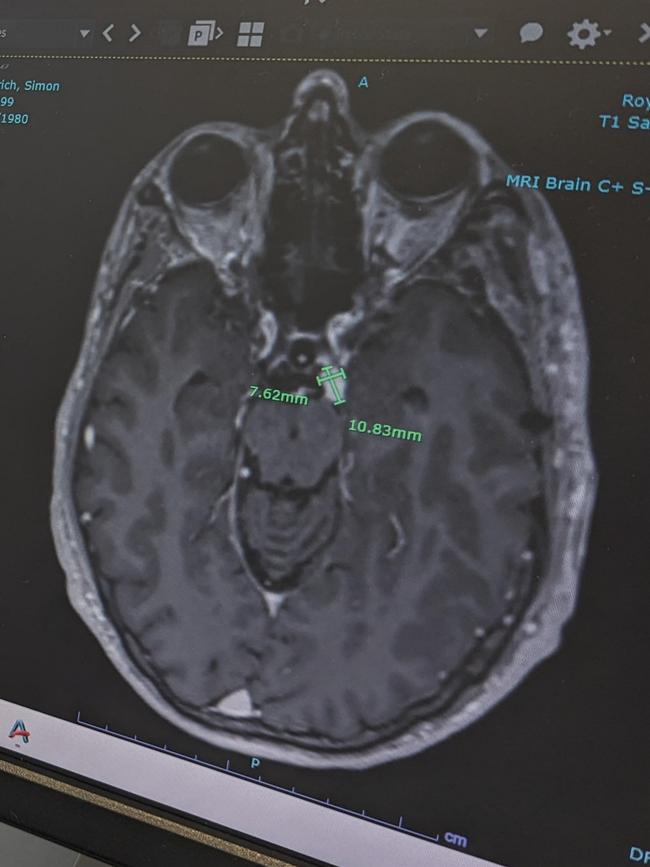
The headaches became so extreme that Simon and his wife were forced to cut their honeymoon short, at which point – after presenting at Emergency on New Year’s Eve – he was diagnosed with a brain tumour the size of a golf ball.
While doctors were able to fully remove Simon’s tumour, he suffered a brain bleed and needed a second surgery the following day, one that left him permanently deaf in his right ear, with constant tinnitus and facial pain he still deals with to this day.

“Nonetheless, I got through it,” says Simon with characteristic resilience. “I was in hospital for two months and had to learn to eat, drink and walk again, but ultimately it looked like the kind of feel-good story people love: young guy, just married, finds a tumour but beats it.
“People were really supportive – and we thought that was it, it was in the past.”
A life-changing diagnosis
And for a while, it was. Until a decade later, Simon began having recurrent back pain.
“I got massages and physio and nothing was working, so I decided I should get an MRI as a precaution,” says Simon.
It was then doctors discovered a series of spinal tumours, and eventually, handed Simon a diagnosis of Von Hippel-Lindau Syndrome (VHL), a genetic condition in which tumours and cysts grow in various parts of the body. These can include the brain, spinal cord, retinas, ears, pancreas, adrenal glands, kidneys and more.
Associate Professor Kathy Tucker is a geneticist, who specialises in rare hereditary cancers. She’s been caring for VHL patients since 1993.
“VHL is a change in a gene,” Dr Tucker explains, “that means that the cell doesn’t have the right mechanism to turn off cell growth. And it’s particularly important in the growth of blood vessels. So it makes blood vessels grow in the wrong places, and basically, the cells get a message that they’re not getting enough oxygen, so they increase blood supply to the region.”
What this meant for Simon was more surgery – something that would continue indefinitely, as his body continued to produce more tumours.
Since his diagnosis in 2016, when he underwent two spinal surgeries for the tumours in his back, Simon has had an additional two brain tumours removed, another spinal tumour removed, and radiation for a brain tumour that was too dangerous to excise surgically.
Sign this petition to make treatment for VHL available on the PBS.


“It’s just this increasing cadence,” says Simon. “Since 2020 I’ve had a surgery every year. And along with the physical challenges, there’s a huge mental load. You think: why is it speeding up? Will I make it through this one unscathed?
“There is death to worry about, sure, but also paralysis, and other lifelong disabilities that I may have to contend with. You can never relax.”
Hope on the horizon – at a cost
A few years ago, Simon became aware of a new drug on the market called WELIREG (marketed as Belzutifan), which has been proven to shrink certain VHL tumours.
Until this point, surgery has been the only option to fight VHL, but Belzutifan now offers another option, and could reduce the trauma of constant surgeries. The catch, however, is that the drug currently costs patients $12,000 per month to access.
“I had heard about the drug’s progress and had been following it for a few years, but for obvious reasons I didn’t think I could pay for it,” says Simon.
But when a brain tumour developed that couldn’t be removed surgically, Simon found himself running out of options.
In the coming months, Belzutifan is up for consideration to be added to the Pharmaceutical Benefits Scheme (PBS). Should the Government decide to add the drug to the PBS, it could be available for as little as $7.70 per month to patients, however there is no guarantee of when or if this will happen.
In the meantime, Simon and his wife made the drastic choice to draw down on their mortgage to pay for the expensive medicine – at least for a little while.
“I really didn’t know what to do, and then I spoke to my cousin, who asked me ‘how much is a life worth?’” he recalls.

“I’m extremely lucky to be able to manage this, and I think it’s so unfair that others can’t access it,” Simon says, adding that he believes it should be made accessible to all VHL patients without delay.
“I’m an unusual case in that I’m the only one in my family with the disease,” says Simon. “For most VHL patients, they have parents, siblings, children with the condition. It’s just not possible to pay $12,000 per month, per patient.”
Simon is now six months into taking the new drug, and every one of his tumours has shrunk by at least 66 per cent.
“The surgeon was absolutely astonished,” he says, “they’d never seen anything like it.”
Simon’s good health news is wrapped in a crippling monthly financial burden, however.
“It’s absolutely not something we can sustain long term and at the moment we’re taking it six months by six months. Even if I can just give myself a year without major surgery, because of this drug.”
At the same time, Simon is keen to use his experience to raise awareness about VHL and Belzutifan to try and secure access for everyone with the brutal disease.
Meredith Cummins, CEO of NeuroEndocrine Australia (NECA) says her organisation is campaigning hard for Belzutifan to be added without delay to the PBS.
“Every person deserves to have their best life and to have fair, rightful options for the
management of their condition,” she says.
“Every person deserves to have quality of life. How can you put a price on a life when considering approving a medication or not?”
Dr Tucker is also hopeful for a swift and positive decision around adding the drug to the PBS.
“Depending on the different cancer, or tumour types, there is between a 50 and 90 per cent chance of it decreasing the tumours,” she says. “So, that’s not just stopping the tumours getting bigger, but actually making them shrink.
“This is the most exciting thing that’s happened for me in my career in terms of being able to turn around the lives of people rather than just screen for things that are going to get worse. Belzutifan has the potential to change outcomes.”
She adds that as well as being life changing in terms of reducing surgeries and the build-up of trauma for patients with this rare condition, the bottom line for the healthcare system is positive as well.
“Even if you think about it purely as a cold hard cost effectiveness thing – if you could avoid the multiple surgeries, you’re not only avoiding the trauma to the patient and the trauma to their bodies, but you’re also saving the healthcare system.”
Add your voice to the campaign to get Belzutifan added to the Pharmaceutical Benefits Scheme (PBS) to reduce its price to as little as $7.70 per month for patients in desperate need. Please take 30 seconds to sign this petition.
Dr Tucker would like to disclose that she’s authored educational material about Belzutifan for MSD Australia.
Originally published as Terrifying reason for groom’s ‘stress headache’




