‘Outrageous’: Parents speak out after baby’s death at Sydney’s Northern Beaches Hospital
The parents of a baby girl who died at a troubled Sydney hospital alleged the death was “completely avoidable”.
Illness
Don't miss out on the headlines from Illness. Followed categories will be added to My News.
The parents of a baby girl who died at Sydney’s troubled Northern Beaches Hospital have shared their “anger and frustration” over the tragedy, alleging time delays contributed to what they believe was the “completely avoidable” death of their daughter.
Sydney couple Leah Pitman and Dustin Atkinson lost their baby daughter, Harper, in February, shortly after a problematic birth.
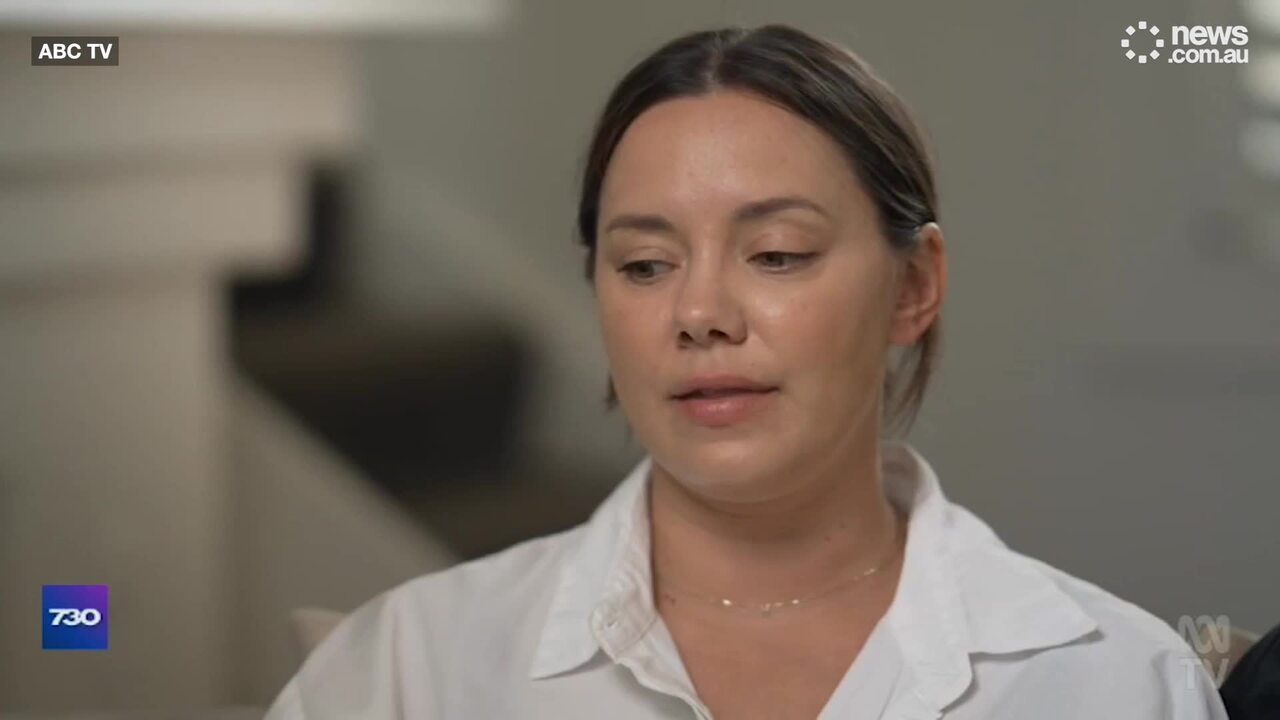
Speaking out for the first time to ABC’s 7.30 on Wednesday night, the pair, who share a young son, said Harper “was let down”.
“We were let down as well, and it’s not fair. We have to carry this for the rest of our lives, knowing that something could have been done to prevent this,” Ms Pitman told the program.
The 34-year-old said she had “a really positive, straightforward experience” when welcoming her son, Ziggy, at Northern Beaches Hospital – which is run as a public-private partnership between the NSW government and Healthscope.
However, while she was at the hospital, she remembers reading about two-year old Joe Massa, who died last September after he received care at Northern Beaches.
“I was actually lying in bed being monitored – I was on my phone and saw the story pop up -and I just remember thinking, ‘Oh, my God, those poor parents, that is so heart-wrenching’, and not knowing what was to come that weekend for us,” she said.

Harper had been conceived through IVF but it was otherwise a low-risk pregnancy, 7.30 reports.
Ms Pitman was booked in to be induced at the hospital on a Friday. However it was postponed to the following day due to staff shortages, according to the program.
She later returned to the hospital on Saturday after going into labour, arriving in the birthing suite at about 8.20pm.
But things immediately went wrong and she began experiencing extreme pain in her lower back.
At about 9.30pm, her waters broke.
“There was blood in my waters. And I just remember looking down at the floor and thinking, ‘Oh God, is that normal?” Ms Pitman recalled.
An hour later, an obstetrician examined Ms Pitman and said he believed she was having a placental abruption. At 10.55pm, he instigated a Category One C-section, which is called when the life of a mother and baby is in immediate danger.

But instead of being taken to the operating theatre, Ms Pitman said they were “left to wait” in the birthing suite.
“I remember asking them, ‘why aren’t we moving, why aren’t we going anywhere?’ We were left in birthing suite, just standing there,” she said.
“They kept explaining, ‘theatre’s not ready. Theatre is not ready’ And I just remember thinking ‘OK, it must be busy’. There must be an operation happening at the moment.”
The pair later learned the hospital has no 24/7 operating theatre. On Friday, Saturday and Sunday nights, the hospital staffs its operating theatre using an on-call arrangement. Staff must live within 30 minutes of the hospital.
“Why is there no 24/7 theatre at a hospital that serves 350,000 people on the northern beaches?” Ms Pitman said.
“It just seems outrageous.”


Harper was unresponsive when she was delivered at 11.52pm – about one hour after the obstetric emergency was called.
“I watched them do CPR on her chest, work on her for what felt like eternity but was minute after minute after minute,” said Mr Atkinson.
It took 21 minutes for Harper to take her first spontaneous breath.
“I actually said to Leah while they were doing the CPR … ‘we’ve lost her, we’re not getting her back after this’. You can’t not breathe for 21 minutes and come out of it unscathed, you know, it’s just impossible,” the 39 year old said.
Early on Sunday morning, Harper was transferred to Sydney’s Royal North Shore hospital.
But hours later, the couple were told the devastating news that Harper would not survive and they made the difficult decision to turn their daughter’s life support off.
“It was just such a horrendous day,” Ms Pitman said.
“She’s been through so much, and she was just such a little trooper. We both just decided ‘we need to do what’s right for her’. And we decided to take her off life support.”
The pair had four hours to hold their daughter before she died, allowing Ms Pitman to have her “first proper skin-to-skin cuddle with her”.
“It was amazing, but also just heartbreaking at the same time, knowing that this was all I was going to have,” she said. “I should have a life of this with her.”

Less than two months on, Ms Pitman said she feels “incredibly angry”.
“I’m obviously sad every single day that she’s not here with us, but so much anger and frustration, knowing that she could be, and that her death, we feel, was completely avoidable.”
The couple allege two failings with the hospital – the delay in the arrival of the obstetrician to the birthing suite and the wait for staff to arrive at the theatre.
“(There were) time delays,” said Ms Pitman, adding “things weren’t urgent enough”.
“Prioritising profit over healthcare. That’s what went wrong,” said Mr Atkinson.
“What they said to us, was it wasn’t economically feasible for them to operate that hospital … with a 24-7 theatre,” he claimed.
He said he had no doubt his daughter would be alive if there was a theatre team ready to assist.
“It is purely the fact that we ended up at Northern Beaches Hospital on the days that their theatre isn’t open 24/7, that cost our daughter her life.”
The Northern Beaches Hospital is conducting a review into Harper’s death.
In a statement provided to news.com.au, Healthscope said it extends its “deepest sympathies and condolences to Leah Pitman and Dustin Atkinson on the loss of their baby Harper”.
“Our clinicians have met with the family to help answer their questions and queries, and a Serious Adverse Event Review (SAER) is currently underway in line with NSW Health policy,” it said.
“We are unable to discuss the details of baby Harper’s case while the SAER is underway. The findings of the review will be shared with the family upon completion and any recommendations or leanings arising from the SAER will be implemented as appropriate.
“The on-call theatre model is not unique to NBH, similar models are in place at a number of other NSW public hospitals, and across Australia. Without exception, all decisions regarding mother and baby were made by clinicians solely based on what they felt was the best treatment for the patient in a rapidly changing set of circumstances. No treatment decisions were made based on anything other than the welfare and safety of baby Harper and her mother.”

Last month, NSW Premier Chris Minns announced a ban on all future public-private partnerships at acute hospitals. He has also prevented future governments from entering into partnerships that could limit control over hospital services.
Known as “Joe’s Law”, the ban ensures critical public services like acute hospitals remain in public hands and are safeguarded from privatisation.
Last week, Healthscope chief executive Tino La Spina acknowledged that operating Northern Beaches Hospital as a public-private partnership was no longer compatible with the government’s objectives.
Mr La Spina said returning Northern Beaches Hospital (NBH) to NSW Health would be best for patients, staff and the community if that was the government’s preferred objective.
“As the state’s appointed operator, we recognise we must work in alignment with the government’s objectives for the health system overall, rather than in conflict with them,” he said.
“The public pressure brought about by the change in policy re. public-private partnership structures has created uncertainty about the NBH future and this has put strain on NBH’s people and operations.
“In the current circumstances, we believe NBH will operate more effectively as part of the public hospital system and its future is assured.”
Originally published as ‘Outrageous’: Parents speak out after baby’s death at Sydney’s Northern Beaches Hospital