ICU plan to cope with Covid surge in NSW hospitals
NSW government modelling indicates Covid ICU cases will surge in October and plans on how the state’s already stretched system will cope is to be revealed.

NSW Coronavirus News
Don't miss out on the headlines from NSW Coronavirus News. Followed categories will be added to My News.
Covid patients requiring ventilation in intensive care units in NSW hospitals have almost doubled in the past 10 days from 32 to 62 with doctors saying they are ‘preparing for battle’ as a predicted surge hits in October.
NSW Premier Gladys Berejiklian and intensive care specialists will outline the plan for how the state’s hospitals will cope on Monday.
The Australian and New Zealand Intensive Care Society (ANZICS) conducted an inventory of the nation’s ICU beds last week, presenting the data to national cabinet on Friday.
The state currently has 39 public intensive care units and 22 private ICUs with access to 2000 ventilators.
The total number of commissioned adult ICU beds as of July 2021 was 592 and as of last week 846 which means Covid cases are taking currently taking up one quarter of available beds.

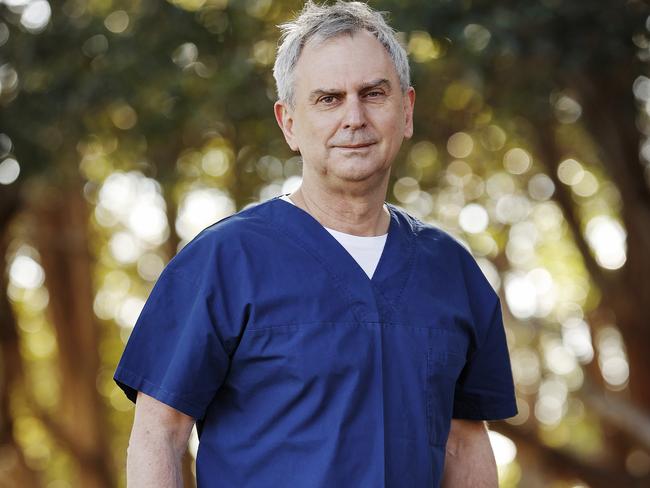
Sydney-based intensive care specialist and vice president of ANZICS Dr Mark Nicholls said they could rise to the challenge by recruiting extra staff from other fields and co-opting wards like surgical recovery and cardiac care as long as the surge was short-lived.
“I know that the teams in each hospital will do whatever they can to deliver the highest quality care to anyone that needs intensive care, but it’s not ideal or sustainable which is why it is really important people get vaccinated as soon as they can. It depends on what the numbers peak at, but with time, people will get tired so I don’t know how long it is sustainable for,” Dr Nicholls said.
ICU staff will be recruited from other specialties Dr Nicholls said.
“You can get up to 100 per cent capacity and still maintain high quality care but you have to pull in resources from other groups from those with similar skills such as anaesthetic staff, but when you do that is it challenging and it is not sustainable in the long term,” he said.
Dr Suzi Nou, President at Australian Society of Anaesthetists, said anaesthetists were already working in ICU wards.
“It feels like we are preparing for battle, but there is lots of discussion about not if but when we will be overwhelmed and by how much,” she said.
NSW Health Minister Brad Hazzard said if intensive care units reached capacity “there would be arrangements to transfer them to another hospital.”
Brett Holmes from the NSW Nurses and Midwives Association said nurses were being freed up from surgery and recovery departments and upskilled to ICU but he said a model of care already in place in Concord Hospital that could roll out across the state was a concern.
“They intend to change the model of care like they have at Concord already where they have moved towards a model of care where the intensive care nurse is left to supervise four other nurses in that upskilled category and relying on the intensive care nurse to spread across the four patients,” Mr Holmes said.

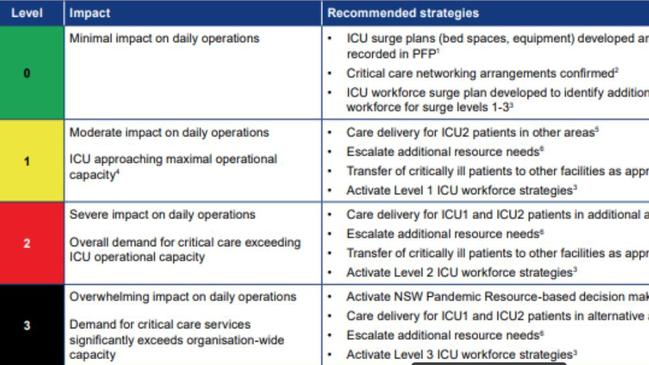
The NSW ICU Pandemic Short Term Escalation Plan has a three step code. For units in stage three where there is “overwhelming impact on operations” where demand exceeds capacity, units are to “Activate NSW Pandemic Resource-based decision making” which means medicos will decide which patients get treated.
“The process of triaging intensive care resources includes both the process of allocating resources and the process of withdrawal of resources, for all patients … it may be necessary at some point to begin prioritising limited critical care resources to those with a need for treatment and those who are most likely to survive,” the guidelines say.
“Making critical decisions about complex situations is something intensive care doctors do very day in consultation with the patient and the family which is something we do in Covid times and non Covid times, people can be reassured this is what we have been trained to do,” Dr Nicholls said.
Vaccination is proven to reduce hospitalisation. 80 per cent of the current 173 in ICU are unvaccinated, and 16 per cent have had one shot.
Got a news tip? Email weekendtele@news.com.au