‘Virus doesn’t wait’: Call for immediate changes to aged care
The head of the Royal Commission into aged care has called on the government to implement “practical” staffing and organisational changes immediately to deal with coronavirus as the pandemic won’t “wait”.
NSW Coronavirus News
Don't miss out on the headlines from NSW Coronavirus News. Followed categories will be added to My News.
- NSW records 18 new cases, new deadliest day for VIC
- COVID vaccine breakthrough as government calls for help
The head of the Royal Commission into aged care has called on the government to implement “practical” staffing and organisational changes immediately to deal with coronavirus as the pandemic won’t “wait”.
Commissioner Tony Pagone QC closed a hearing focused on the impact of COVID-19 on residential aged care by urging the Morrison Government to “listen” to warnings from experts.


“We’ve heard of a number of very helpful suggestions in the course of the hearing by people who have had direct experience and a great deal of personal expertise,” he said.
“We can only urge government to listen to that carefully.”
“The virus doesn’t wait, and nor should the measures that need to be implemented to deal with the virus wait either.”
Mr Pagone said while the Commission was “not in a position” to make recommendations at this early stage, but pointed to several measures that could be addressed now.
“Dedicated aged care specific national co-ordinating body to advise government, such things as additional staff so as to enable greater visitation in aged care homes so that the informal care that is missing can take place, these are all practical things that should perhaps not wait,” he said.
Mr Pagone said it had been hard to gain an understanding of the impact of the coronavirus while it was still “playing out around us”.
“That has been very difficult indeed,” he said.
Health Minister Greg Hunt today responded by defended the government’s spending on aged care, but would not say if more money would be given to the sector to deal with major staffing issues before the end of the Royal Commission.
“We’ve provided an injection of $850 million to assist with a mixture of staffing, infection control, preparedness support, in addition to that we have provided the Victorian Aged Care Response Centre,” he said.
“The separate element of (staff) ratios is of course a matter that the Royal Commission is dealing with, but absolutely the key lesson here from around the world is that community transmission drives the impact on aged care.”
Mr Hunt said 0.1 per cent of aged care residents in Australia had died from coronavirus, which was a 50 times lower rate than in the UK.
“Every life lost is an agony, so we’re going to fight for every life,” he said.
Earlier today the commission heard, in its final submission, that Australia’s top government authorities and aged care providers failed to do “all that could be done” to save the lives of 220 aged care residents who died during the COVID-19 pandemic.
Senior counsel assisting the inquiry Peter Rozen QC said key parts of the government’s plan for curtailing COVID-19 in aged care were “plainly wrong”.
“Not all that could be done was done. The sector was not properly prepared in March before the Dorothy Henderson and Newmarch house outbreaks. The lessons of those outbreaks were not conveyed to the sector … And the sector is not prepared now,” Mr Rozen said.
“Another lesson that does not appear to have been learnt is that providers should prepare to lose close to their entire workforce in the first few days of an outbreak. The figure of 20-30 per cent … is plainly wrong. It should now be confined to the dustbin of history.
“Our elderly citizens and their families deserve better.”
Mr Rozen concluded that masks should have been made compulsory earlier in the pandemic and the 56-page government document detailing the government’s response was “a plan, just not an aged care plan”.
“It does not take great insight to see that having three to four different groups in authority to make a decision is going to create confusion,” he said.
“Remarkably the first two versions (of the CDNA doc) made no mention of the federal government having a role in the system, that it funds to the total exclusion of the states.
“Whatever else may be said about the documents they are not the comprehensive plan of a regulator facing the COVID-19 pandemic.”
Mr Rozen said none of the problems that faced the aged care sector during the pandemic were unforeseeable.
AGED CARE HOMES ASSESSED THEMSELVES AT HIGH LEVEL
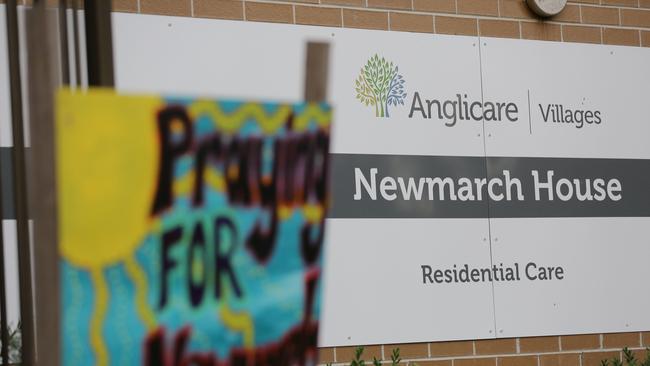
On Wednesday, the commission heard that more than 40 per cent of Australia’s aged care providers, including the virus hit Newmarch House, ranked their facilities as “best practice” before the COVID-19 pandemic – despite workers reporting gross breaches of hygiene, neglect of residents and staffing issues.
Aged Care Quality and Safety Commissioner Janet Anderson told the Aged Care Royal Commission that she was not surprised by the large degree of confidence among providers but the commission is now implementing more regulatory measures.
“We have become more questioning and we have deployed a number of additional regulatory activities in order to both prompt activity or action by providers,” Ms Anderson said.
Newmarch House in Western Sydney, where 17 people died from COVID-19, also ranked itself as “best practice” in an industry self-assessment survey.

The ACQSC chief clinical adviser Dr Melanie Wroth said she advocated for COVID positive patients at Newmarch House to be separated from the facility.
“Having spoken to the staff at Newmarch house and understanding the difficulties that they were experiencing … I was advocating that as one of the options,” she told the commission.
“The best way to protect people as happens in the general community is that you completely limit the exposure of people who may still be negative from having any contact with people who tested positive.”
Health Secretary Dr Brendan Murphy defended the government’s decision to not make masks compulsory in Victorian aged care homes until July 13 despite community transmission rising since June.

But Dr Murphy conceded that in hindsight, earlier use of masks could have possibly saved lives.
“(It) could have been implemented earlier, absolutely.”
Defending the government’s management of COVID-19 in aged care Dr Murphy said data which showed that 68 per cent of COVID deaths in the country were in age care, was a “meaningless statistic”.
“I would like to strongly reject the assertion that somehow the proportion of an extraordinary low death rate has any pejorative meaning,” he said.
“We have detected, identified, and transparently reported every single aged care case of COVID. Many high-income countries didn’t even bother to report aged care deaths.
“We have an 11 per cent death date in ICU with COVID one of the lowest in the world. This is a completely meaningless statistic.”

Meanwhile, a “plan” for responding to COVID-19 in aged care written by the federal government only warned homes to plan for losing up to 30 per cent of their staff, well below the workforce shortages experienced in major outbreaks.
The commission heard residential facilities with COVID-19 lost considerably more staff, including Newmarch House which lost about 84 per cent, but at the start of the pandemic providers were only advised by the government to prepare for 20 to 30 per cent losses.
Deputy Secretary for Ageing and Aged Care Michael Lye said the government believed its own “rapid response” surge workforce would be best placed to boost staffing levels in residential homes with COVID-19 outbreaks rather than expect the providers to prepare.
Mr Lye then conceded it was “unrealistic” to expect workforce losses that low.
Prof Murphy added it was felt to be “unrealistic” to expect providers to cover more than up to 30 per cent of their workforce without outside help.
Commonwealth officials were grilled by counsel assisting the commission Peter Rozen QC in a series of awkward and confusing exchanges about how the government helped aged care providers prepare for COVID-19.

At the start of the hearing the Commission denied a request by Prof Murphy to respond to claims the federal government did not have a plan for COVID-19 in the sector.
Prof Murphy requested the “indulgence” to address claims by Rozen QC in his opening address, which said the Commonwealth did not have a plan for COVID-19 and aged care.
His attempt to respond to the claims was considered out of order and he was able to make a written submission on the issue.
Mr Lye also defended Australia’s death rate in aged care, where about 0.1 per cent of the population in facilities have died – a much lower rate than other countries such as the UK.

Meanwhile, the commission also heard that health workers looking after the state’s vulnerable elderly have reported incredible breaches of infection control, rife under staffing, and “abject neglect” of residents.
In April, during the peak of the pandemic’s first wave, just 29 per cent of Australian Nurses and Midwifery Federation workers reported that their PPE was adequate, evidence presented to the Royal Commission showed.
ANMF Federal Secretary Annie Butler said the union raised the urgent need for more staff and training with Aged Care Minister Richard Colbeck on March 4 but did not get a meeting until April 4.
“We had members tell us they could only use one glove rather than two. We had members who told they had to reuse equipment, put it in collective plastic bags. A whole range of incredible breaches in infection control,” Ms Butler said.
“We requested a meeting with the Minister from 4 March. We didn’t get a meeting until 4 April despite insistence and despite raising our concerns.”
Health Workers Union secretary Diana Asmar said workers “feel like they are on the bottom of the Titanic Ship.”
Ms Asmar said no briefings were given to aged care workers in Victoria as they grapple with the rising second wave.
“Our workers are traumatised. They were shocked that they didn’t get any precautions about what’s happening, any communications. They weren’t even told how to deal with these situations,” she said.
“We came to situation where there was no soap, no sanitisers for them, the actual masks were locked up in medication cupboards.
“Until today in the aged sector, our members still cannot get masks, gloves, gowns. Today with a huge outbreak in Victoria, with these death tolls, our members are struggling to get a mask.”
Monash University head of Health Law and Ageing Professor Joseph Ibrahim said Australian aged care residents were treated as “second class citizens” throughout the pandemic.
“This is the worst disaster that is still unfolding before my eyes and is the worst I’ve seen in my entire career. I didn’t think we would sink any lower following the Royal Commission finding last year,” Prof Ibrahim said.
“We failed because we’ve treated residents as second-class citizens. There is an absence of accountability and there is no consequences for failing to deliver good care in aged care.
“In my opinion, hundreds of residents are and will die prematurely, because people have failed to act.”
Elderly Australians made up 68 per cent of deaths from COVID-19 so far.
Prof Ibrahim said a lack of clear outlines on which health authorities were leading the pandemic response contributed to the poor outcome.

“We don’t divide an emergency into different little bits. You don’t manage a disaster by consensus.”
The key witnesses to the commission added that he had advised the government in April to put Australian Defence Force personnel into aged care centres to monitor the COVID-19 response.
NSW Health ministry deputy secretary Nigel Lyons said the authorities did not remove COVID-19 positive residents from Newmarch House based on expert medical advice that it was not yet clear how many had the virus.
“It was a strong view that we should leave people in place until it became clearer in terms of the extent of the outbreak,” Mr Lyons said.
“The strong advice we had was that at this point in the outbreak it was very difficult to actually know who was COVID positive. You couldn’t be definitive that people were COVID negative because it may be that they are incubating the virus.
“(It was the view) that we should actually leave people in place at this point in time until it became clearer as to the extent of the outbreak.”
