Hospital’s plea to MP: End unfair scan price pain
Patients are being put at risk for the sake of “frustrating” penny-pinching red tape that has left a major Brisbane hospital’s state-of-the-art $2m MRI scanner hamstrung. | SIGN THE PETITION FOR CHEAPER MRIs
North
Don't miss out on the headlines from North. Followed categories will be added to My News.
PATIENTS are being put at risk for the sake of “frustrating” penny-pinching red tape that has left a major hospital’s state-of-the-art $2m MRI scanner hamstrung.
The private, not-for-profit St Andrew’s War Memorial Hospital, at Spring Hill, is facing off against healthcare providers across the nation, all competing for just 20 licences that will allow them to claim the full Medicare rebate for MRI scans.

General manager Wally Bourdelov said he was “extremely frustrated” with the licencing scenario, which was putting patients at risk and causing them unnecessary pain. At present the hospital has a partial licence, leaving patients with the difficult choice of paying higher out-of-pocket costs for an MRI, or travelling to another facility that can offer a fully subsidised scan for all Medicare-eligible conditions.
SIGN THE ST ANDREW’S WAR MEMORIAL PETITION HERE
“I am frustrated on behalf of our patients,” Mr Bourdelov said. “The services we provide are covered properly in all areas, but the one thing missing is the licence for our MRI.”
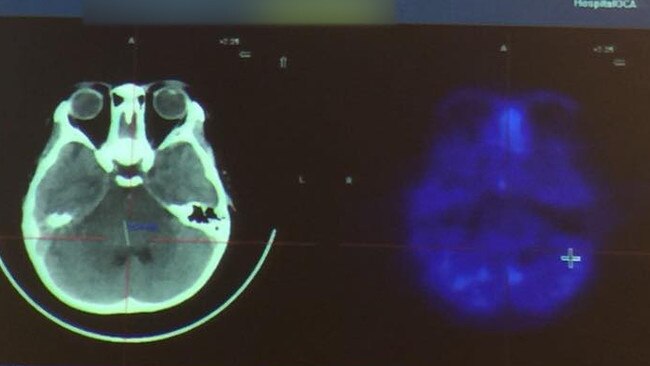
Orthopaedic surgeon Dale Rimmington said MRI was indispensable when diagnosing soft-tissue injury, as it gave more accurate information than other imaging, such as x-ray or CT, and without harmful radiation.
“Cost is a big thing for patients,” Dr Rimmington said. “It’s very difficult to get by without readily accessible, affordable MRIs.”
PAIN IN THE POCKET
THE Federal Government’s competitive MRI licencing bid is causing real pain for patients.
Orthopaedic surgeon Dale Rimmington, who operates at St Andrew’s War Memorial Hospital at Spring Hill, said the lack of a full Medicare MRI licence at the hospital meant patients often had to choose between paying more or hobbling to another provider to find a more affordable MRI scan.
“Yes … it can cause a patient pain if they have to be subjected to being put on a stretcher and into an ambulance and transferred to somewhere else,” he said.
“It has happened to me where a patient decided against getting scan in hospital while an in-patient because of the cost. It wasn’t something that was critical at that minute, but in my subspecialty that doesn’t happen very often.
MORE:
Shorten’s MRI plan clouded by costly rollout in 2011
No more rebates for GO-ordered knee MRIs for over 50s

“But if it happened to one of the spinal surgeons, that could have a big impact on the patient and really potentially have a detrimental effect on their outcome if they had to travel with an unstable spinal injury or something like that. It is very important.”
Mr Bourdelov said it was a “ridiculous situation” that the sixth largest hospital in Queensland — with more than 250 beds, a busy emergency department plus a world-class neurology service — did not have a full licence. Brisbane Private Hospital, also located at Spring Hill, has had a full licence for their Brisbane Private Imaging-operated MRI machine since 2016.
“We are a private hospital one of the highest acuity levels in the State — the degree of sickness and emergency care provided — vastly higher than hospital down the road, yet we do not have an MRI licence but they do,” Mr Bourdelov said.
MRI licences were handed out to 10 hospitals last month but none in Brisbane, even though the Federal Government’s own figures show the city has among the lowest access rates in the country.
The licencing regime was reformed after a Federal Inquiry into the cost of medical imaging, which also recommended sweeping changes to what conditions were covered, including banning some scans based on the age of the patient.
Mr Bourdelov said St Andrew’s was the first private hospital to have an MRI machine, in 1990. He said if the hospital were to receive a full licence “there will be no out of pocket costs for Medicare rebatable MRIs for both in-patients and outpatients at St Andrew’s”.
The fees imaging services charge for scans are not regulated by the government.
PEOPLE POWER: HOW YOU CAN HELP:
Sign the petition here
Write to Federal Health Minister Greg Hunt and explain why you think St Andrew’s Hospital should receive a full Medicare licence for their MRI machine. Please be sure to provide a contact name and phone number for verification purposes.
Email: Minister.Hunt@health.gov.au
or via post PO Box 647, Somerville, VIC, 3912

CASE STUDY
CONFUSION over MRI bulk-billing is a real pain for patients, and that doesn’t just mean to the hip pocket.
Clayfield father Luciano Bastian Machado (pictured) said he was teaching his daughter to climb on monkey bars at a Toombul park when he fell and badly injured his knee last week.
While doctors suspected he had done major damage to tendons, he had to endure six painful extra car trips travelling to hospital, a GP and then to an imaging service for a scan. The keen jogger said he also had to take extra time off work.
“I was lying on the ground in pain (at the park) and another father there — I didn’t know him — drove me home,” he said. “I went to the Royal Brisbane Hospital emergency department, where the doctor said I had probably injured my tendons and would need an MRI.” The doctor told him that if a GP wrote a referral for a scan, it was likely to be bulk-billed.
However, that is not the case, as Mr Bastian Machado found out. His GP was reluctant to write a referral for an MRI scan, due to cost.
But, Mr Bastian Machado insisted and he chose St Andrew’s because he had previously used their imaging department.
“It has cost me about $260 — but that cost is added to the gap I paid at my GP, which was around $50, which I will have to pay again for the result.”
And that also means more painful car trips, folding his damaged knee into and out of a car and using crutches to get around.
If Mr Bastian Machado had have bypassed the public system and gone straight to St Andrew’s emergency department, he would have paid an out-of-pocket fee of about $200. If the hospital had a full MRI licence, the scan would have been bulk-billed and could have been performed on the same day. He would have then been referred to a specialist at St Andrew’s, if further treatment was necessary.

WHAT IS MRI?
■ MRI: Magnetic Resonance Imaging.
It uses magnetic fields to provide very detailed pictures of the body.
■ Why is it expensive?
Machines cost more than $1.5 million; St Andrew’s estimates it costs about $100,000pa just to keep it technologically up to date. Operators must be specially trained.
■ Why are there Medicare licences for MRI scans?
Federal Health Department: “MRI is a sophisticated technology. Since its introduction to the Medicare Benefits Schedule (MBS), MRI has been managed with careful consideration of requester, provider and item level needs. These needs continue to direct the provision of high quality, safe and cost-effective health care in Australia.”
RESPONSE FROM HEALTH MINISTER
City North News send a number of questions to Federal Health Minister Greg Hunt.
This response was sent from a spokeswoman for the Federal Department of Health:
■ On 23 September 2018 the Government announced nine new locations would be allocated Medicare eligibility for magnetic resonance imaging (MRI) services. This is in addition to Medicare eligibility for the Kalgoorlie Health Campus which was announced on 22 June 2018.
■ The 10 locations were identified from requests made to the Government for MRI access. Consideration was given to a number of factors such as:
— the relative need of the Primary Health Network (PHN) in which the hospital or service was located (based on the number of Medicare eligible MRI units per 100,000 population, the time lag between specialist referral and rendering of the service, availability of operational machines and distance to eligible machines); and

— alignment with investments made by public and private hospitals in MRI technology and health infrastructure, providing access to patients at hospital facilities.
■ While none of the initial 10 locations identified are in Brisbane, the Pindara Private Hospital on the Gold Coast is included for an upgrade.
■ On 24 September 2018 a competitive Invitation to Apply (ITA) process opened to allocate a further 20 additional MRI units access to Medicare, which closes at 5pm (Canberra time) on 2 November 2018.
■ The criteria for assessment includes mandatory and substantive criteria, which are included in the ITA document available on the Department’s website www.health.gov.au/diagnosticimaging.
■ On completion of the ITA assessment process, the Department will provide an assessment report to the Minister for Health.
■ The Department will contact successful applicants after they have been selected to enable commencement of Medicare eligible MRI services from as early as 1 March 2019.
■ A Medicare-eligible MRI machine does not guarantee patients won’t have out-of-pocket costs as providers are free to set their own fees and these may exceed the fees set out in the Medicare Benefits Schedule.
■ No additional rounds for expansion, after this ITA, have been announced.
Here are the questions asked by City North News of the Health Minister:
How many applications have been received thus far?
How many of those are from Brisbane?
When would the licences be given out?
Will the gap-payment policy of each potential licence holder be considered when deciding the licence allocation?
Would facilities who pledge to charge low or no gap be given preference for a licence?
Is the age or technological capability of the MRI machine taken into consideration when a licence application is assessed?
Is there likely to be another round of licences released?
Is there an avenue for appeal if an organisation is not granted a licence?
When would the licences have to be renewed? Would the organisations have to reapply for the licence at that time?
Under what conditions would a licence be taken away (after being granted)?
Currently, what checks are made on the effectiveness/quality/technological capability of existing licenced machines by the licence issuer?
Could the Minister please respond to criticism that the list of 10 Licences already granted does not include one from Brisbane, even though the city has the third and fourth lowest MRI per 100,000 people (Brisbane North, Brisbane South).
(Reference: https://www.greghunt.com.au/400000-australians-to-access-lifesaving-medicare-scans/ http://www.health.gov.au/internet/main/publishing.nsf/Content/diagnosticimaging-expansion-of-medicare-eligible-magnetic-resonance-imaging)
Criticism has been levelled at this licencing process from various sources (according to media reports), as being too mired in red tape; limiting competition in the sector and therefore keeping prices high; and not addressing the need for more scans for more ailments to be included in the lists of those qualifying for Medicare rebates. Can the Minister please comment on the value of this licensing process, in terms of improving quality of care for Australians?
.
Greg Hunt’s media release on September 24, 2018
More than 400,000 Australians will now be able to access lifesaving scans for cancer, stroke, heart and other medical conditions with a $175 million investment from the Morrison Government.
Patients in 30 additional locations right around Australia will now be able to access MRI scans when they need it under Medicare.
An MRI is a commonly used medical scan which gives a detailed view of the soft tissues of the body such as muscles, ligaments, brain tissue, discs and blood vessels.
It is used by doctors to diagnose and monitor a number of different medical conditions including cancer, cardiac conditions, trauma and sporting injuries.
The Liberal National Government is helping Australians stay healthy while keeping the cost of healthcare down for families.
Our plan for a strong economy means we continue to deliver record funding for essential services such as Medicare, public hospitals and life-saving medicines.
Today we announce the first ten locations to receive this new Medicare support, including;
Mount Druitt Hospital, New South Wales
Sale Hospital, Victoria
Royal Darwin Hospital, Northern Territory
Mount Barker, South Australia
Pindara Private Hospital, Gold Coast, Queensland
Northern Beaches Hospital, New South Wales
Toowoomba Hospital, Queensland
Monash Children’s Hospital, Clayton Victoria
St John of God Midland Public and Private Hospital, Western Australia
Kalgoorlie Health Campus, Western Australia
Each of these sites has been identified as a location of critical patient need. In many cases hospitals already have this technology ready to provide services from 1 November 2018.
The Morrison Government is committed to providing high quality health services when and where they are needed.
Not only will our new Medicare support ensure patients get the most appropriate treatment and save money, it will also cut down the amount of time patients have to spend travelling to get a scan.
Medicare subsidised MRIs will be accessible in these locations from 1 November 2018, subject to the sites meeting the required approvals and administrative requirements.
Tomorrow we will open a competitive public application process for the location for a further 20 Medicare eligible MRIs and we invite prospective facilities to apply for consideration.
The Morrison Government’s additional 30 sites will bring the total number of fully Medicare eligible MRI machines to 204, a more than 17 per cent increase across Australia.
Earlier this year we boosted Medicare support for a new MRI scan for prostate cancer checks helping 26,000 men each year, as well as a new Medicare listing for 3D breast cancer checks, helping around 240,000 women each year.
Medicare spending is guaranteed and increasing every year from approximately $24 billion in 2017‑18 to $28.8 billion in 2021‑22.
The Liberal National Government has also announced an additional $2 billion investment in diagnostic imaging over the next decade.
We are retaining the bulk-billing incentive and indexing targeted diagnostic imaging services including mammography, fluoroscopy, CT scans and interventional procedures.
By contrast, Labor has only committed $80 million and not made any commitment to the re-indexation of diagnostic imaging rebates.
24 September 2018


