Young mum Ashley Evans denied insurance policy payout for vital ovarian mass surgery
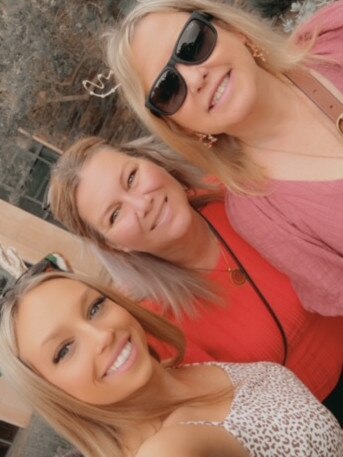
Young mum and cancer survivor Ashley Evans has been handed a devastating blow with her health insurer refusing to pay for surgery after the discovery of a huge ovarian mass.

SA News
Don't miss out on the headlines from SA News. Followed categories will be added to My News.
Single mum Ashley Evans is embroiled in a health insurance battle as she lives with debilitating pain from a growing ovarian mass.
Diagnosed with an orange-sized lump on her ovary in November 2023, Ms Evans has been denied health insurance coverage for the surgery she needs to remove it.
“It has been scary … I’ve had some days were I’ve fainted at work, I just push through the pain,” she said.
“I never know when I’m gonna stop feeling dizzy … I can’t eat a lot because if I eat a lot it (the mass) puts too much pressure on my stomach and the pain gets worse.
“I went from 65 kilos to 42 in a month.”
Her pain is made more traumatising by the fact she recently recovered from cervical cancer only months before.

In April 2023, Ms Evans was told she had cervical cancer after she presented at the Women’s and Children’s Hospital in excruciating pain.
“I was quite emotional, I was scared … I’m so young and I was told it would lessen my chances of being able to have any more kids,” she said.
Prior to the Lletz procedure Ms Evans had to remove her cancer in June, she underwent a range of scans, including scans on her ovaries which showed no health concerns.
The surgery was successful, however the following month Ms Evans, who works as a repairs specialist, continued to have abdominal pain and received a referral to see a specialist oncologist to ensure her cancer hadn’t returned.
That was when she decided to take out Bupa health insurance in September.
“I wanted to (sign up) in case I did end up needing a hysterectomy,” she said.
A few months later, after a range of tests and scans, doctors told the Salisbury North mum they found a 5cm mass on her right ovary and she needed surgery.
“I wasn’t expecting a phone call to say that I had a mass on my ovary so that was devastating especially not knowing, still even to this day, whether it’s a cyst or whether it’s a tumour,” Ms Evans said.

Unfortunately her health insurance told her they wouldn’t cover the surgery.
“I found out Bupa were going to classify it as a pre-existing condition based off symptoms rather than covering it,” she said.
“My daughter’s birthday is three days before Christmas and I found out on her birthday.
“I’ve had another referral to go through the public system so I am on the waiting list for that but unfortunately … we are not sure how long it would take before I could even get seen by them.”

Ms Evans said Bupa denied her coverage because they classified her ovarian mass as a pre-existing condition despite May 2023 scans, completed prior to getting health insurance, showed her ovaries were clear of any health concerns.
“I signed up (to Bupa) in September and I didn’t see my oncologist until October but because the referral was put through a month before I signed up and … I had the symptoms prior to signing up, even though my scan showed nothing wrong with my ovaries at that time … they’re trying to say that it was already there before I signed up,” she said.

Ms Evans, who is a single mum to six-year-old Charlotte, must continue to work through her constant and nauseating pain.
“I need the money to help me get through and pay all my bills so not working would put me in a really bad position,” she said.
She said without insurance coverage she will be out of pocket $20,000 at least for the surgery.
A Bupa spokesperson said “Bupa empathises with the challenging situation faced by our customer, however we are unable to publicly comment on the specifics of any individual’s case, for privacy reasons”.
“In general, when customers take out their health insurance policies, we advise them of waiting periods relevant to their policy. Pre-existing conditions are defined by the Private Health Insurance Act as being those where signs of symptoms were present during the six-month period prior to joining or upgrading their cover,” they said.
“When assessing if a condition is pre-existing, our medical practitioner who makes the decision must take into account information provided by our customer’s treating doctor.
“Customers are invited to provide additional medical information for a second review of their medical history for a further review of their case.”
If you’d like to donate to Ashley, you can here.
Following inquiries from The Advertiser Ms Evans received an email from Bupa on Tuesday confirming they will cover her surgery to remove the ovarian mass.
Bupa has been contacted for comment.
More Coverage
Originally published as Young mum Ashley Evans denied insurance policy payout for vital ovarian mass surgery





