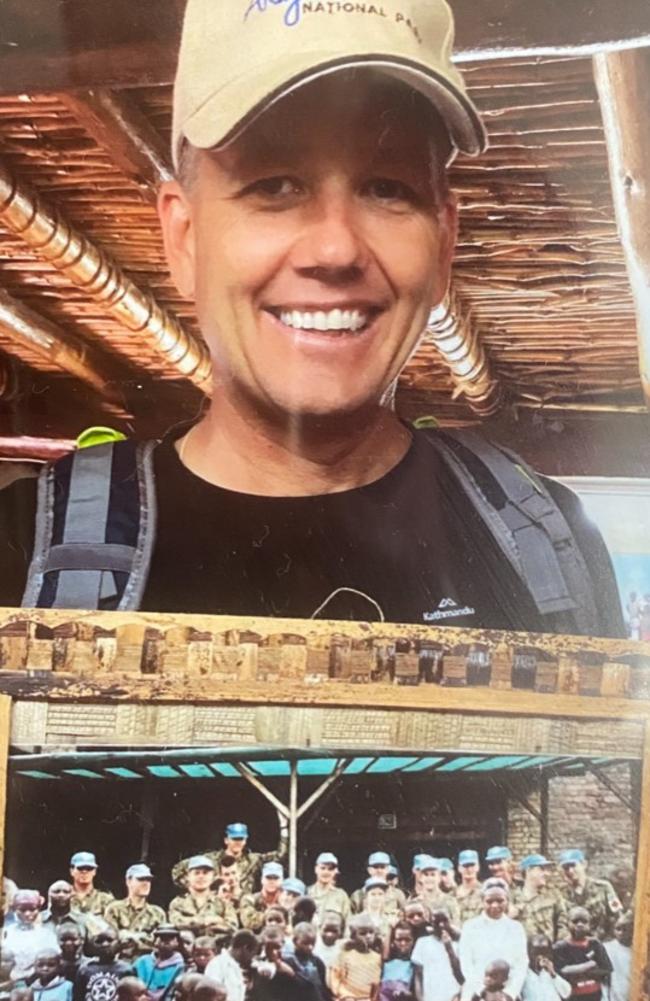
Miles Wootten advocates for modalities to heal PTSD
An ex-serviceman who was “rocked to the core” from his time as a peacekeeper in Rwanda says more support is needed for veterans recovering from PTSD when they return from war.

Noosa
Don't miss out on the headlines from Noosa. Followed categories will be added to My News.
A Buderim nurse and a former Australian Army soldier are calling for broader support for the mental health of current and former servicemen and women this Anzac Day.
A registered nurse at a repatriation hospital in Melbourne for more than 30 years and now a clinical nurse consultant in pain management, Claire Dunkley has been treating ex-peacekeeper Miles Wootten, 50, for more than five years.
Mr Wootten was experiencing insomnia, depression, involuntary outbursts of anger and ongoing reflux problems when he met Ms Dunkley at a personal development course in Melbourne.
“When I first met him, he couldn’t work,” Ms Dunkley said.
“It was like he got back, did his thing and then they just forget about them.”

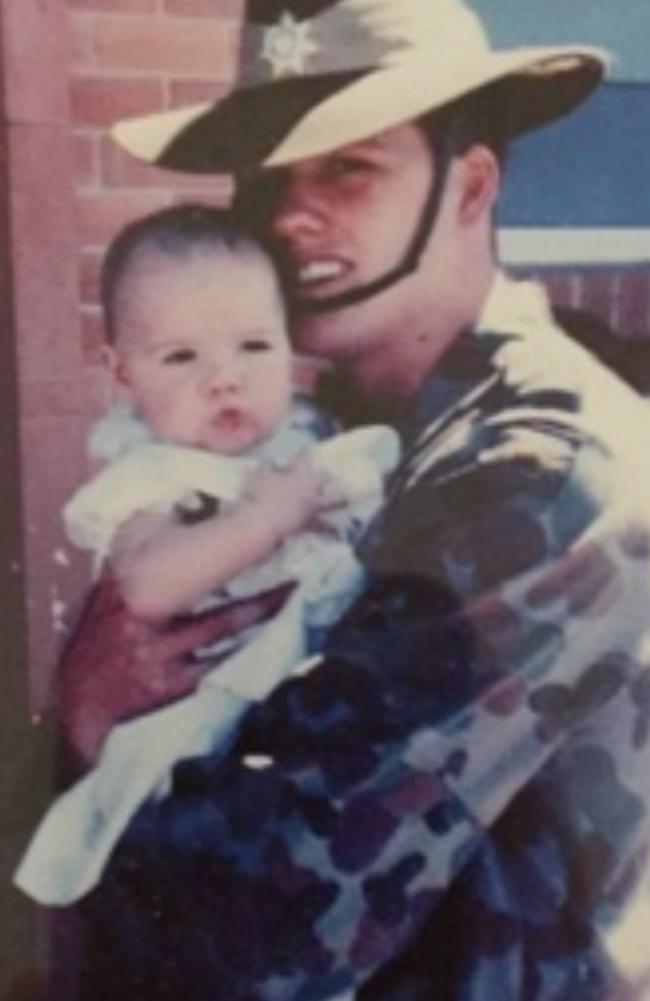
Mr Wootten was deployed as a Peacekeeper Officer to Rwanda when he was 21 “to clean up the damage of the Civil War as part of the Advance party”.
From August 1994 to February 1995, aged 21, he worked as an Army driver and was also given the job of scrubbing down rooms in the morgue.
“Seeing the devastation of people, lives, blood and gore rocked me to my core; it was truly a living hell to see humans suffering to an extent I could never have imagined,” Mr Wootten said.

Ms Dunkley began treating Mr Wootten in 2018 for late onset Post Traumatic Stress Disorder symptoms from her private pain-treatment centre Cluzie Clinic in Buderim.
“My grandfather was in the second world war and became an alcoholic and passed away from liver disease because of all of that,” Ms Dunkley said.
“I’ve always been able to listen to people’s horrific stories.”

Using Aminoneurofrequency Therapy to “reboot the person’s nervous system”, Cluzie Clinic primarily helps people with stress-related disorders.
“It’s a bit like acupuncture except without needles,” Mr Wootten said.
“There are little patches you wear on your skin for three days and it will do it’s thing, so it talks to your nervous system to get it back to what it should be doing.
“And the best part about it is that you only use it when you need it, so it’s not like a repeat prescription, for me it’s just when things flare up.”
Ms Dunkley also uses breathing exercises, “grounding in nature” and emphasises the importance of “talking to someone”.
“Miles was ignored for years, and he suffered in ways no hero should,” Ms Dunkley said.
“For the extreme trauma he went through, the person he has become now is someone you would really want to admire.”

Mr Wootten says his ability to focus on the positives of his time in Rwanda has helped with his healing.
“To put yourself in harms way to protect someone you don’t know – that’s the stuff I would gladly do again,” he said.
“To feed people that are starving, to give water to people who have nothing, to help with basic things, to look them in the eye and give them a hug and do whatever.”
Mr Wootten says he is open to different modalities and believes the Department of Veterans’ Affairs need to support veterans seeking alternative avenues for healing.
“With companies like Claire, the DVA are really taking the slow approach, they still have an antiquated way at looking at healing,” he said.
“They’re only just starting to cover new therapies and there needs to be a lot more ease of funding.
“They need to take away the red tape and look at it logically to just make it easier.”
A Department of Veterans’ Affairs spokesman said the Department had a “duty of care” to veterans and their families to fund treatments proved to be effective, safe and compliant with legislation.
“Under the legislation, DVA may only fund treatments with extensive clinical evidence of effectiveness and safety,” the spokesman said.
The spokesman said the Department did not comment on details of an individual’s case “for privacy reasons”.
“DVA continuously monitors the latest medical evidence to ensure veterans have access to the best available treatments for their mental and physical health needs,” the spokesman said.
“There are many established PTSD treatments available that have demonstrated effectiveness and known safety.”
Services funded by the Department included psychiatrists, GPs, pharmaceuticals and other community-based programs.
“This care is free and is available to anyone with a single day of continuous full-time service in the Australian Defence Force,” the spokesman said.
“We encourage any veteran who may be experiencing trauma or mental health concerns to engage with Open Arms – Veterans and Families Counselling, who are available 24/7 on 1800 011 046.”