Medical society lodges protests about AHPRA investigations after doctor suicides
A Queensland-based medical professional society is challenging AHPRA after 16 practitioner suicides in four years, citing 10,000 complaints of persecution and stressful investigations.
QLD News
Don't miss out on the headlines from QLD News. Followed categories will be added to My News.
The suicide deaths of 16 medical practitioners in four years has prompted a Queensland-based professional association to challenge the nation’s medical watchdog.
Queensland-based Australian Medical Professionals’ Society, AMPS, has lodged complaints and submissions with two investigations underway into the Australian Health Practitioner Regulation Agency.
The professional representative body made its submissions after receiving more than 10,000 complaints from doctors and the public who claim AHPRA persecuted them or they were subjected to stressful and lengthy investigations.
AMPS lodged submissions with the National Health Practitioner Ombudsman review in October and with the Independent review of complexity in the National Registration and Accreditation Scheme review in November on behalf of its 700 members.
Suicides, stress leave, illnesses, marriage breakdowns and loss of income are some of the horrifying side-effects AMPS has documented about Queensland doctors who had undergone AHPRA investigations.
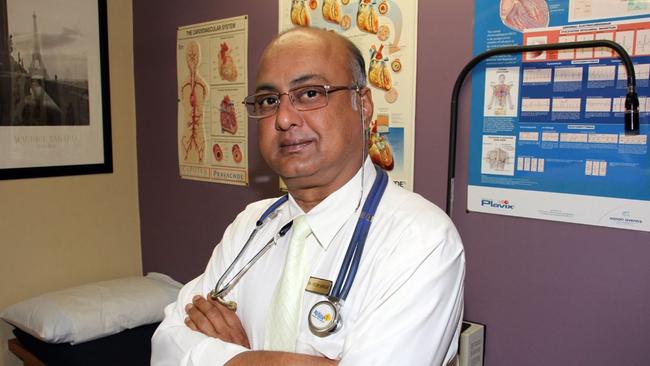
This week, Brisbane-based Dr Prem Adhar said he was forced into early retirement after a six-year battle with AHPRA and Queensland’s Dr Melissa McCann is currently awaiting an outcome from QCAT after her stance on the government’s Covid response.
Buderim gastroenterologist Dr Andrew McIntyre spent five years and more than $20,000 to clear his name and was recently investigated again with no further action.
Melbourne’s Dr Jereth Kok was suspended for five years for professional misconduct because of his online stance on abortion and gender. He has retrained but is still awaiting VCAT’s decision on his career which is not expected until mid 2025.
Dr Duncan Syme was suspended in February 2022 after he wrote temporary exemption letters for patients with severe psychological distress and Dr Paul Oosterhuis challenged a 2021 NSW Medical council decision and later won his case.

Submissions were sent to the two investigations after AMPS sent its complaints to both AHPRA and the Office of the Health Ombudsman, which both recommended forwarding the complaints to the review panels.
AMPS secretary Kara Thomas said the society’s submissions claimed AHPRA regulations had been “weaponised” and investigation processes were taking a severe toll with 20 practitioners attempting suicide since 2019.
The 16 deaths were documented in the International Journal for Quality in Health Care in September 2023 in a report into AHPRA and practitioner distress, which include contributions from retiring AHPRA CEO Martin Fletcher.
That report found 20 incidents with 16 resulting in death, 12 confirmed suicides and the remaining four were listed as “suspected suicides”.

Eight of the practitioners were doctors, eight were nurses and four were other healthcare practitioners.
The National Health Practitioner Ombudsman review into AHPRA was initiated in June after the deaths were reported and a rise in complaints from doctors.
The country’s Health Ministers set up an independent review in May into the complexity of the National Registration Scheme, which is under AHPRA’s stewardship.
Both reviews follow a 2020 Senate Community Affairs References Committee’s Inquiry into AHPRA, which has since taken steps to address the way it handles complaints, notifications, and investigations.
Ms Thomas said her organisation made its submissions after an outpouring of anger and distress from doctors, including 20 from Queensland, who had been suspended or who stopped practising.
She said a survey of 1018 medical practitioners this year found 52.2 per cent had been investigated by AHPRA with a staggering 78.5 per cent of those, claiming they had been unfairly treated.
The survey also found 51.6 per cent of those who had interactions with AHPRA rated their experience as 0 out of 10, with the average rating a mere 1.7 out of 10.

Respondents were also asked if they believed AHPRA’s processes were fair and transparent in dealing with complaints with 989 respondents, answering ‘No’.
The survey also found widespread concern about AHPRA’s handling of vexatious and anonymous complaints with many practitioners reporting lengthy, stressful investigations based on unfounded or malicious grievances, often with little recourse.
“This is creating a climate of fear and defensiveness among healthcare professionals, potentially impacting patient care,” Ms Thomas said.
“The lack of adherence by AHPRA to legislative time frames and clear, consistent communication during investigations further exacerbates these issues.
“Many practitioners question the value they receive from AHPRA given the high and increasing registration fees.
“It is leading to a major health crisis not only for the public but for our doctors as well.”
The submissions called on both reviews to recommend a comprehensive overhaul of AHPRA’s policies, practices, and organisational structure and the implementation of a more efficient, fair, and transparent complaints process.

Retiring AHPRA and National Boards chief executive Martin Fletcher, who will step down from his role next month, responded to AMPS complaints and told the society to submit them to the two reviews already underway.
“The independent review of complexity into the National Registration and Accreditation Scheme headed by former Health Complaints Commissioner of New South Wales Sue Dawson is currently consulting on a range of topics related to the National Registration and Accreditation Scheme, including the system of complaints about registered health practitioners,” he wrote in a letter.
“Given this review is underway and active, I recommend providing feedback to Ms Dawson and her review team for their consideration in considering options to improve the complaints system.
“We understand Ms Dawson will provide a report to Health Ministers with recommendations in the first half of 2025.”
AHPRA was contacted for a statement.
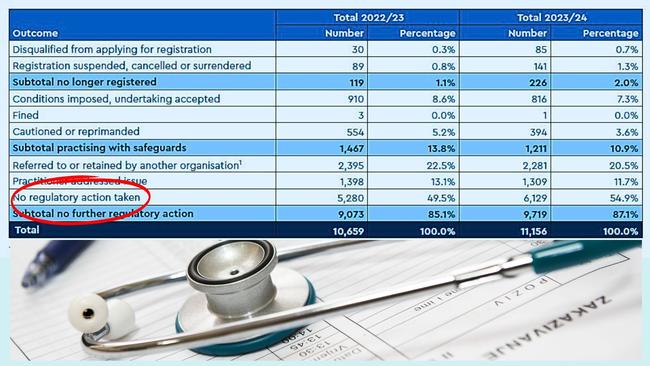
In its annual report tabled last week, the authority said it had made major progress in the way it handled complaints over the past year.
It also said it had established a team to support improved consultation with health complaints organisations in each state and territory.
“As a result, consultations between AHPRA and the organisations were completed an average of 7.6 days sooner than in 2023.
“AHPRA also worked with the Medical Board of Australia and Dental Board of Australia to streamline decision making for lower-risk concerns, which resulted in a 33-day reduction in the time to complete lower-risk matters.
“Nearly 80 per cent of all finalised notifications were closed within six months of receipt with 45.1 per cent (5029 complaints) within three months of receipt, and a further 34.5 per cent (3849) three to six months from receipt.”
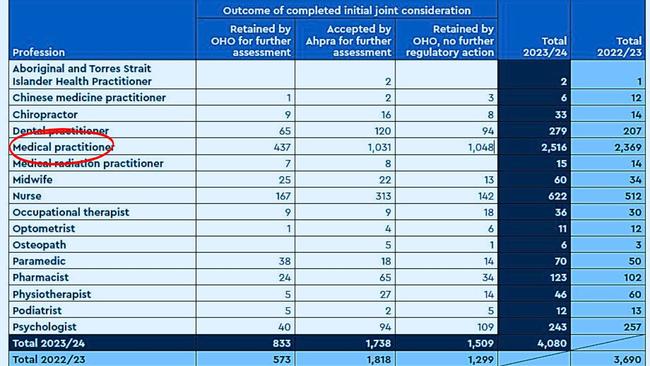
AHPRA and the Office of the Health Ombudsman responded to 4080 notifications in Queensland in the 2023-24 year with 42.6 per cent referred to both AHPRA and the National Boards to manage.
A National Health Practitioner Ombudsman spokeswoman also recommended AMPS’ documented concerns be sent to the two reviews.
“I acknowledge the concerns you have raised … about the Australian Health Practitioner Regulation Agency (AHPRA’s) conduct and regulatory framework,” the spokeswoman said in a letter.
“I also acknowledge the concerns you raised about medical practitioners’ experience of the notification process, arising from a recent survey about AHPRA conducted by the AMPS.
“Any practitioner is welcome to contact us directly to raise any specific concerns they may have about the handling of their regulatory matter.”
Ms Dawson’s independent review is due to table its final report, findings and any recommendations to Health Ministers in April.





