Mackay Base Hospital rolls out new measures to combat soaring bed crisis
The Mackay Base Hospital is taking steps to combat an occupancy rate problem that is poised to get worse, with data revealing the number of people waiting on stretchers before being seen in the emergency department.

Mackay
Don't miss out on the headlines from Mackay. Followed categories will be added to My News.
The Mackay Base Hospital is resorting to extraordinary measures to free up beds as they tackle a 100 per cent occupancy rate only poised to get worse.
MBH chief medical officer Dr Charles Pain reveals they have created a new Rapid Access paediatric clinic and converted the Patient Travel waiting room into a Transit Lounge for patients nearing release who do not require physical beds.
He said they had also introduced the statewide “transfer initiative” nursing role, which can see patients imported into the hospital via paramedics so ambulances can be “released”.
New data shows about three in 10 patients who presented to the hospital’s ED from October to December waited on a stretcher for 30 minutes or more.
This figure was compared to almost four in 10 at Bundaberg Hospital, and one in 10 at Townsville University Hospital.

The revelations about Mackay’s moves to free up beds follow Health Minister Yvette D’Ath’s comments Queensland’s public hospitals were meant to work on a “very small margin of bed capacity”.
“No hospital sits there with a large empty bed capacity,” Ms D’Ath said during her visit to Rockhampton last week.
“If you’re doing that, you’re not running your hospital system efficiently.”
New data released this week from Queensland Health reveals a substantial rise in the number of patients staying longer than 24 hours in emergency departments.
Across the Mackay HHS, 157 patients remained in ED for more than 24 hours in the 2015-16 year.
For 2021-22, the number had jumped to 478.
For 2022-23 year-to-date, the number is 491.
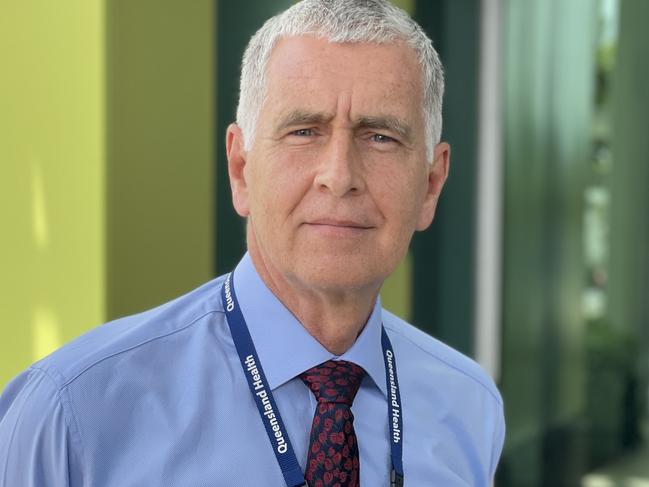
Dr Pain said MBH, which will receive 128 extra beds in late 2026 under a $250 million expansion, was “very busy” and facing twin pressure points of population growth and an increasing complexity of cases.
He said the nationwide “phenomenon” was partly due to an ageing population but also chronic diseases like diabetes, “quite a lot of presentations with suicidal attempts or suicidal ideations”, and psychiatric illness.
He said “at the other end of the spectrum”, people were presenting to hospital emergency departments who could instead visit GPs or other clinicians for emergency needs like stitches.
Dr Pain said work was being done across the state to increase the health system’s capacity outside of hospitals, but Mackay’s shortage of bulk-
billing GPs was partly a roadblock to that end.
There were 13,347 patients seen at MBH’s ED from October to December, new data reveals, with 90 per cent seen within clinically-recommended times.
But only 57 per cent on average were in and out of the ED within four hours, a figure Dr Pain would like to see rise to 80 per cent.
“Hospitals and hospital beds are a very precious resource, we have to manage those as well as we can,” he said.
Dr Pain said the MBH would like to be at 85 to 90 per cent bed capacity, rather than its current 100 per cent.
“I just really want to reassure people that we run a good hospital here,” Dr Pain said.
“We have wonderful, very good, committed staff here with a highly-skilled workforce.




