How high cost medical devices are driving health fund premiums up
Funds are blaming the high cost of medical devices including stainless steel bolts for adding around $200 a year to private health fund insurance costs.
National
Don't miss out on the headlines from National. Followed categories will be added to My News.
- Common medicines could lead to cancer patients’ deaths
- Aged care Rich Listers ‘worth $342m’ as sector cries poor
It measures just 8mm but a tiny bolt that costs a staggering $1023 is one of a multitude of medical devices including sponges and glues driving up your health fund premiums.
Health funds claim the combined effect of these miscellaneous charges is adding $1,000 to the cost of a standard knee or hip replacement.
And it is undermining a deal reached by the federal government that was meant to save health fund members $1.1 billion by bringing medical device prices here into line with cheaper prices in Europe. Instead, it’s adding as much as $200 a year to private health premiums.
News Corp can reveal health fund members are paying $1,023 for a stainless steel bolt used multiple times in an external leg brace when a competitor product costs $45 and a similar bolt costs just $2.64 at Bunnings.
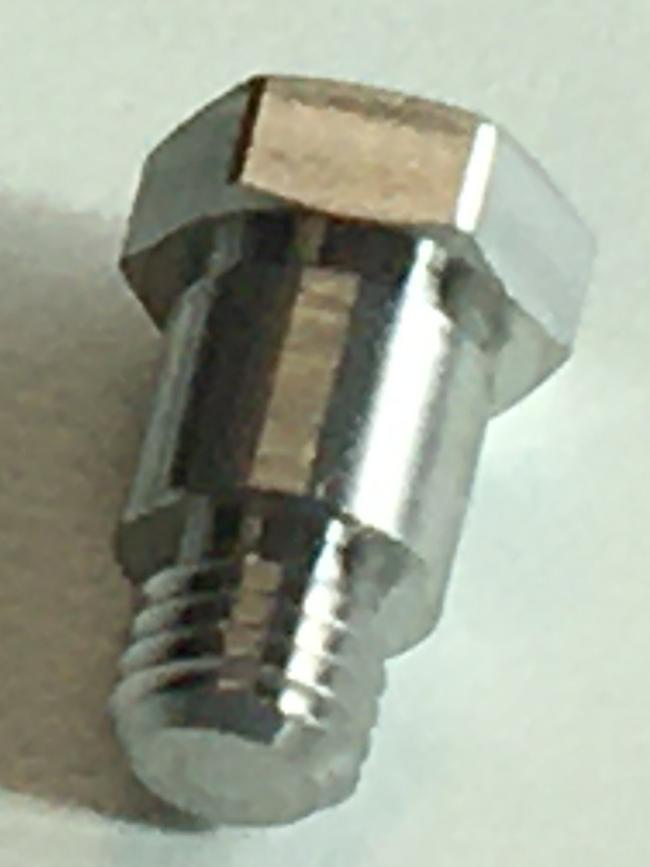

The high cost bolt can nearly quadruple the cost of the procedure that fixes bone deformities in children and adults and helps manage injuries caused by trauma from $15,000 to $57,000.
Australian Medical Association president and orthopaedic surgeon Dr Omar Khorshid said the cost of the bolt was “ inexplicable”.
“That’s either a mistake or it’s, you know, smart companies being sneaky about how they price their products, I don’t know, the explanation for it,” Dr Khorshid said.

The federal government sets the prices health funds must pay for medical devices and its committee approved the $1,023 price.
Health funds have raised an objection to the price but are still waiting six months on for the outcome of a price review.
Medical device company Johnson & Johnson Medical said “we will accept whatever determination is made by the Department of Health with respect to how MaxFrame and its individual elements should be classified.”

Orthopaedic surgeons are increasingly using a $1,443 tube of surgical sealant called Evicel that is only approved for use in high risk bloody heart and brain operations.
There has been a 359 per cent growth in the use of this sealant since 2012-13 and its driving up the cost health fund premiums.
In one instance, more than $10,000 of the sealant was used in a single knee replacement surgery.

Johnson & Johnson said “the circumstance described is likely to have involved a patient suffering a significant uncontrolled bleeding episode in which case the use of fibrin sealant may have saved a life or a limb”.
The company also said Evicel has three indications:
1. For all patients undergoing surgery where standard surgical techniques are considered insufficient and provides sustained haemostasis for intraoperative bleeding when control of bleeding by standard surgical techniques (such as suture, ligature or cautery) is ineffective or impractical.
2. As suture support for haemostasis in large vessel vascular surgery.
3. For suture line sealing in dura mater closure.
Dr Khorshid said there may be very rare examples where there is uncontrollable bleeding to use the glue in orthopaedic surgery but if surgeons were using it routinely it “would appropriately be questioned by the profession”.
A surgical sponge called Nasopore is also adding pressure to premiums. It costs health fund members $143 per unit while it sells online and for $US39.99 ($AUS55.61).
A spokesman for Stryker said “we note that instances of NasoPore being sold online to the public for USD$39.99, are where retailers are selling expired products which is a practice that Stryker does not condone.
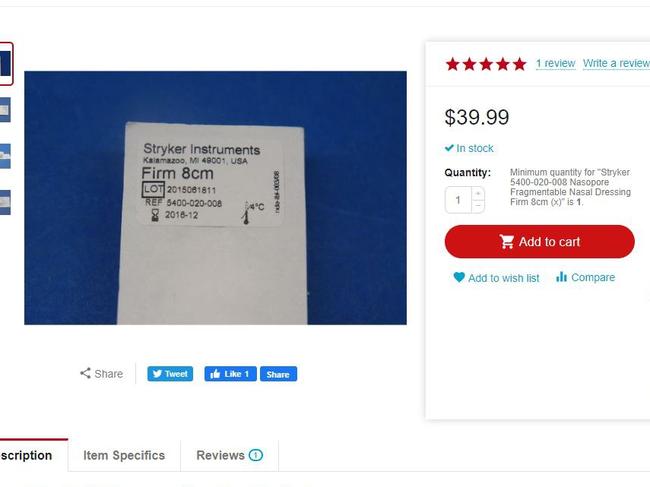
Stryker categorically rejects any claims that NasoPore is responsible for increasing private health insurance premiums.
The total spend on NasoPore in 2018-19 amounted to 0.08 per cent of the approximately AU$2.1billion (APRA) spent on all prostheses in Australia; and 0.007 per cent of the AU$25.3 billion annual revenue (APRA) of private health funds in that same year.”

In 2016, the Federal Government claimed it was saving health fund members $1b by slashing the price health funds had to pay for hip and knee replacement devices.
However, instead of falling by $1b medical devices costs have soared by $23.9m as medical device companies make up for the lost income by charging more for sponges and bolts.
“It just happened as a way of clawing back the value that they lost when the government, reduced the price of the unit price of hip, knee, hips, knees lenses and cardiac implants as part of the MTI agreement,” Private Healthcare Australia CEO Dr Rachel David said.


Former health department chief now consultant for the Grattan Institute Professor Stephen Duckett agrees.
“What we’ve seen is the price cuts haven’t worked,” he said.
“The amount that has gone out the door from health insurance has remained roughly the same it just shows that the hospital surgeons or device manufacturers are getting around the cuts by creative billing,” he said.
MORE NEWS
Crucial drug shortage fears as medicines stuck on boats

