Pregnant mum’s life or death decision and her dramatic world-first surgery
A young Queensland mum has had to face the most difficult of choices: surgery to save her own life or a never-before-tried option that could also save her unborn baby?

QWeekend
Don't miss out on the headlines from QWeekend. Followed categories will be added to My News.
Peter Tesar is home alone in Brisbane, staring trance-like at the ceiling. One of Australia’s leading heart surgeons, he mentally rehearses the operation dozens of times before the real thing, practising every tiny movement, every incision. It’s a ritual the veteran of about 12,000 operations goes through leading up to every complex surgery, something he likens to elite athletes visualising a winning performance to prepare their bodies for success. Olympic divers, he says, imagine every twist and turn, every tuck, well before they begin their climb to the top of the 10m tower.
But for Tesar, in his mid-sixties, there’s much more at stake than an Olympic gold medal. In a few weeks, he’ll have the beating heart of a young woman in his hands, the life of her unborn child dependent on his skill. The surgery he’s about to attempt has never been tried on a pregnant woman anywhere in the world.

Jasmine Rolon already has one child, Raphael and, unexpectedly, is pregnant with her second. Her doctors are worried.
The then 21 year old from Caboolture, north of Brisbane, has a ticking time bomb inside her chest. Rolon has Marfan syndrome, a genetic disorder of the connective tissue, affecting about one in 5000 people. Those with the condition are characteristically tall and slender, with long arms and legs. They frequently have issues with their eyes and bones, but it’s how the disorder affects their hearts that is life-threatening.
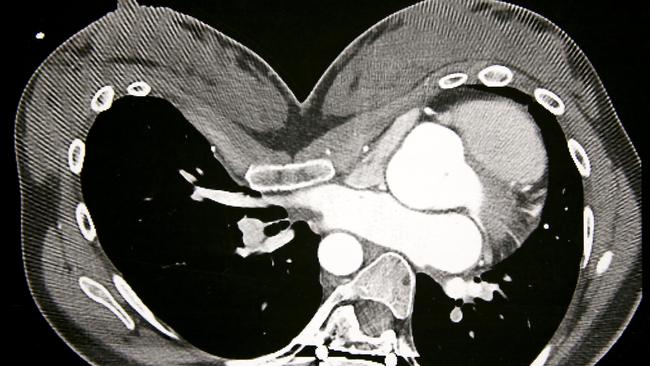
The heart is essentially a living pump. In its centre is a piece of pipe known as the aortic root, which dilates in Marfan patients, putting them in danger of a fatal rupture as they age. Tesar describes it as a bit like a balloon becoming increasingly likely to pop the more air that’s blown into it.
Women with Marfan syndrome are particularly vulnerable while pregnant. Higher levels of the hormone relaxin are produced, softening the aortic root and causing it to stretch further. The risk of it tearing or bursting mounts with each pregnancy. Rolon’s aortic root has grown to 4.7cm in diameter. In most adults, it’s about 3cm.
If she lived almost anywhere else in the world, including the US, Rolon would have faced an agonising choice. She could continue with her pregnancy, putting her own life in jeopardy, and potentially leaving her son, who was still a baby, to grow up without a mother. Or she could be placed on a heart-lung machine, her body temperature lowered to 18 degrees Celsius, for an operation to replace her aortic root with artificial tubing, and probably the aortic valve as well, swapping it with a man-made alternative. Doctors must stop the heart temporarily during the surgery, which lasts about six hours. But that would have meant the almost certain loss of the child she was carrying and a lifelong reliance on anticoagulant medication.

In Queensland, Rolon had a third option. At The Prince Charles Hospital, in the northern Brisbane suburb of Chermside, a 40km drive south from Rolon’s home, Tesar and colleague Dr Livia Williams, had just introduced an alternative operation, dubbed the PEARS procedure – an acronym for Personalised External Aortic Root Support. Most PEARS surgery is performed without the need for a heart-lung machine, giving the young mum the chance to save her unborn baby. But with the operation never having been performed on a pregnant woman before, there were no guarantees.
“I was kind of like: ‘I don’t know what the hell is going to happen here’,” Rolon says. “I could have easily pulled out at any time. But I had to really stick to my guns. I had to weigh up the pros and cons and, obviously, PEARS was the best option. For me, it was like the cycle of life had to continue. I’ve got to do this for my baby.”
Her surgery could not have come at a more stressful time for Rolon’s family who were grieving the death of her younger brother, Jesse. The much-loved 15 year old died suddenly on Anzac Day last year.
Rolon was acutely aware of how much worry she had created leading up to the operation on top of Jesse’s loss. “It was awful,” she says through tears. “That was the hardest bit for me.” But at the same time, the mature young woman, who lives by the mantra “Be Positive”, knew she had to remain upbeat for the sake of the life she was carrying inside her.
“Feeling sorry for yourself does nothing for you,” Rolon says. “I was pregnant with a little baby that’s going to be feeling what I’m feeling. Obviously in your head, maybe subconsciously, you’ve got all these emotions but I was trying to actively not feel that. I’ve worked hard to make myself relaxed. If you stress, it really is felt by everyone around you. I just kept telling myself it was all going to work out, it was all going to be good.”
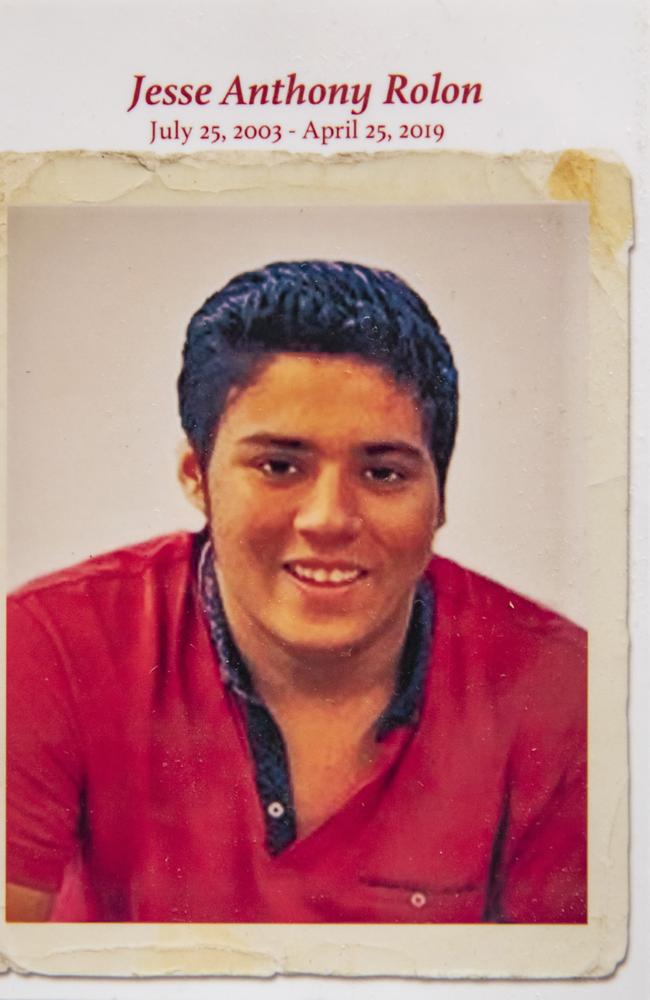
A picture of Jesse sits on a hallway table in the entrance to Rolon’s home. Just days after his funeral, Rolon nervously told her Mum Gabriela Clarkson of her surprise pregnancy. Her first child, Raphael, was not yet six months old. It was Mother’s Day, 2019.
“She was scared to say something,” Clarkson recalls. “It came at a difficult time. But it was beautiful. It was the best news in the world because who wouldn’t want more life when we’d just lost somebody so precious?”
Nevertheless, mixed with the joy for Clarkson was the worry for her only daughter and how her heart would cope with a second pregnancy. At that stage, the possibility of the PEARS procedure had not been raised.
Clarkson only learned of Rolon’s plan to have the surgery once the decision had already been made. She had no choice but to trust her independent, headstrong first-born and put her faith in a surgical team she had never met.
“Jasmine always said to me: ‘The PEARS people are so good, Mum. We don’t need to worry. I’ve asked all the questions. They’ve told me everything I need to know’,” Clarkson says. “She’s so informed in everything. She’s over the top in her investigations and was very much: ‘I know what I’m doing’.”
Almost 350 PEARS procedures have been carried out in 10 countries at 28 surgical centres since the first in the United Kingdom in 2004, including 20 at The Prince Charles Hospital. Eight have also been performed at the Queensland Children’s Hospital in South Brisbane.
Queensland is the only Australian state with a formal PEARS program, although three of the procedures have been done in Melbourne. The concept is relatively straightforward – 3D printing technology is used to create a model of the weakened section of aorta, based on detailed CT scans. A made-to-measure polyester mesh sleeve is then fashioned to fit over the patient’s aortic root and valve, fortifying the at-risk areas. Simply put, it’s a plumbing fix – rather than replacing a leaky pipe, it’s bolstered with scaffolding. In this case, the mesh becomes incorporated into the outside wall of the aorta, strengthening the main artery that supplies oxygen-rich blood to the rest of the body.
Hailed as a major advance in heart surgery, the idea for the PEARS procedure came not from a doctor, but from British engineer, Tal Golesworthy, who has Marfan syndrome himself. When Golesworthy learned he required aortic root replacement surgery or face an increasing risk of premature death, he was unimpressed with what was on offer, particularly the prospect of spending his life on blood-thinning drugs. There had to be a better way, he thought.
In a case of patient heal thyself, he came up with the idea for the PEARS implant, built a technical team, raised capital and became the guinea pig for the first operation in May, 2004, performed by Professor John Pepper at London’s Royal Brompton Hospital.
Now 63, Golesworthy, has been working on the PEARS project for 20 years after a previous background in coal combustion research and development. He’s the technical director of Exstent Ltd, a small medical engineering company based in Tewkesbury, Gloucestershire, where the mesh implants are manufactured. The idea for the material used in the PEARS implant came from knowledge he gained during his coal industry days working with fabric filters.

Golesworthy’s invention has undoubtedly changed lives, including his own. But speaking by email from Gloucestershire, his frustration is evident. Remaining committed to the project to help others has taken a personal toll.
“I frequently say to others involved in PEARS, how I wish they could have met me 20 years ago when I was a happy-go-lucky engineer involved in interesting R and D rather than a burnt-out, worried old wreck,” he writes. Had he known how much “blood, sweat, tears and grief” the journey would entail, he says he may never have embarked on it in the first place. “Of course, when I started … I was selfishly focused on fixing myself,” Golesworthy says. “Unfortunately, I’ve spent over 20 years committed to this project out of a sense of responsibility to my fellow travellers. A laudable endeavour but one that has demanded a significant price from me.”
Innovation in medicine is a painfully slow process, the surgical profession renowned for its conservatism. The acceptance of new procedures can take years, often decades, and is governed by regulation to protect patient safety.
Golesworthy has had to be extremely patient, initially “entirely ignorant” of how stubborn to change many surgeons can be and the stringent rules they operate under. But two decades on from his original idea, as more surgeons embrace the PEARS procedure with accumulating evidence of its effectiveness and safety profile, the company he created is preparing to expand. “With a bit of luck, I will be able to reduce my workload and focus on those parts of the business that I enjoy,” he says.
The Prince Charles Hospital started a PEARS program in March last year with Tesar, its former director of cardiothoracic surgery, at the helm. Tesar wears a scrub hat like a painter’s beret, wielding a scalpel with as much skill as the French masters had with their brushstrokes. He’s an expert in aortic surgery and while the concept behind the PEARS procedure is relatively simple, the technical challenges of fitting the implant over the aortic root and valve while the heart is still beating, are enormous. “The PEARS procedure itself is an operation for the few,” he says without a hint of arrogance. “Not every surgeon should do it. To evolve this as a patient option, it’s important to leave it to a few teams that develop the expertise to do it well, safely, with low mortality risk.”
Jasmine Rolon was about 14 weeks’ pregnant when she was wheeled into the operating theatre for the two-hour procedure in July, 2019. Her case posed significant difficulties, not the least being she was expecting a baby.

Dr Livia Williams, one of just two female heart surgeons in Queensland and herself mum to a toddler, assisted Tesar in the world-first surgery. Accessing Rolon’s aorta to perform the procedure was particularly demanding. Because of her Marfan syndrome, Rolon had what’s known medically as a pectus excavartum – her breastbone was sunken into her chest. The severity of her condition made the PEARS procedure particularly complex from an anatomical perspective. Typically, the heart sits in the centre of the chest, slightly to the left of the breastbone. In Rolon’s case, it was “completely displaced to the left chest cavity”. “The view was very poor,” Williams says. Instead of being able to operate looking down onto the heart after sawing through the sternum, they had to lift up one side of the bone and operate looking in from the side.
Williams did not enter medical school to become a surgeon. Her first dream was to join Medecins Sans Frontieres, Doctors Without Borders, to perform humanitarian work. At age 20, she took a year off medicine to live in Narsapur, a village in India, collecting data as part of a study into factors contributing to stillbirth and deaths among babies in the early weeks of life. But after returning to Melbourne’s Monash Medical School, the former student of Pimlico State High School in Townsville, was hooked on surgery from the moment she first entered an operating theatre. “I felt at ease,” she says. “I just really enjoyed operating, the physical act of operating.”

Now in her 30s, Williams has been a cardiothoracic consultant since 2016, choosing heart surgery because of the intricate, technical nature of the work, describing the complexity as “very intellectually satisfying”. “For this type of surgery, the needle that you use to do the operation is smaller than your eyelash and the suture is thinner than a strand of hair,” she says, borrowing a quote from a fellow heart surgeon.
“I enjoy the intensity, the fact that decisions have to be made extremely quickly in the operating theatre and events can happen suddenly. You have to draw on a huge amount of experience within a couple of seconds to salvage situations.” She went into heart surgery despite it remaining, even in 21st-century Australia, largely a male domain, growing up in a household where she was encouraged to follow whatever career path she wanted.
Under Tesar’s guidance, Williams is being trained to take over the PEARS program once he inevitably hangs up his scrubs. With the program well established at The Prince Charles Hospital – Queensland’s premier public heart treatment facility – Tesar and Williams share the load of being prime surgeon. But they only ever perform the procedure while both surgeons are in the operating theatre, one assisting the other. “We never do it when one of us is out of town,” Tesar says. “It’s only ever done as a complete team, because that gives you the safety margin that the process is done as perfectly as we can make it.”

Rolon’s surgery was planned in detail beforehand. “Like every good operation, you’ve actually done it 100 times before you enter the operating theatre … contemplating all the movement systems, going through all the phases of play, including options for variation, according to need,” Tesar says. They had to change how they would typically operate to account for the anatomical challenges of their patient. Instead of performing the procedure with the two specialists facing each other across the operating table, they worked side-by-side.
Surgeons, like many elite sportsmen and women, have their routines. Tennis great Rafael Nadal avoids walking on the lines of the tennis court before and after every point. Tesar only enters the operating theatre once the patient is prepped and draped. The ritual is part of how he “dissociates”, allowing him to focus solely on the complex job ahead. “Everything’s mapped out,” he says. “How you gear yourself towards making sure you are getting that little bit of set-up angst within you so you know you’re keyed in, it’s all planned.”
The temperature of the operating theatre is set at 17.9C. “People have actually shown that mental performance is greater when it’s a bit cooler,” Tesar explains “You actually design the environment for maximum performance.”
Under the extreme stress of an operating theatre, independent of how unflappable surgeons may appear externally, studies have found their heart rates generally jump to around 150-170 beats per minute – the average adult’s resting heart rate is between 60-100 beats per minute. Even in highly-pressurised surgical situations, Tesar appears calm, his voice measured. His demeanour is one of his surgical strategies for optimal outcomes.
“When you’re running an operating theatre, if the prime surgeon is not calm, then people in tense situations will lose their cool,” he says. “During the high-risk components of operations, you make it quiet. When you give orders or requests, everything is done with a soft tone. It means people have to concentrate but also, it doesn’t stress people.”

Rolon went into the surgery not knowing whether her unborn baby would still be alive when she woke up. She had to sign a consent form allowing her doctors to switch her to a heart-lung machine during the procedure if necessary – a scenario that would have meant the almost certain loss of her child. Still, she knew the PEARS procedure offered the best chance of saving both their lives. As it turned out, Tesar says, the operation went “mostly” to plan. It was only towards the end of the surgery they struck the biggest problem: they were unable to close her chest without her blood pressure dropping – a result of her pectus excavartum. In a dramatic, but successful, end to the operation, they drew on the expertise of another cardiothoracic surgeon at The Prince Charles Hospital, Dr Rishen Naidoo, who had to break bones to realign Rolon’s rib cage, allowing her chest plate to be closed.
It would be five days before Rolon knew her baby was safe. As she lay in The Prince Charles Hospital’s intensive care unit recovering from the surgery, in pain and struggling to sleep, the normally “chilled” young woman’s mind wandered. “In my head, I was like: ‘Maybe my baby’s dead’,” she says. “That was when it was stressful. Your brain goes everywhere. My Mum was coming to see me every day but I wasn’t telling her that was happening because I didn’t want to make anyone sad.”
It wasn’t until Rolon had an ultrasound after leaving ICU, allowing her to hear the thump, thump, thump of her baby’s heartbeat, she was able to finally relax. “I was like: ‘Oh my God, thank God, my baby’s alive,” Rolon recalls. “Everything was normal.”

And here she is, baby Luna, snuggled in her mother’s arms. About five months after Rolon’s world-first surgery, Luna was born by caesarean section at the Royal Brisbane and Women’s Hospital on December 20 – her family’s ultimate Christmas gift. The little girl, described by her Mum as “my miracle baby”, was four weeks early but weighed a healthy 3165g.
Rolon, who turns 23 in October, recently returned with Luna to The Prince Charles Hospital for an appointment with her surgical team. “You look good,” Tesar says. “You’ve come through all this pretty much unscathed. Is it hard having two?” he asks. “Sometimes,” she replies. “But I have very relaxed babies.”
“Life goes on, which is how it should be,” Tesar says. “We’re actually itinerants in people’s lives. What should happen if things go well is that we leave and people then live their life, not live their disease.”
“Thank you very much,” Rolon replies, cuddling her daughter. “Just live,” Tesar tells her. ■
* To donate to heart research at The Prince Charles Hospital Foundation: thecommongood.org.au
