“I couldn’t fathom losing another baby”: Miracle surgery after mum’s double tragedy
After the tragedy of losing two babies with spina bifida, incredible in-womb surgery at the Mater Mothers’ Hospital delivered a miracle. WARNING: GRAPHIC IMAGES
QWeekend
Don't miss out on the headlines from QWeekend. Followed categories will be added to My News.
It’s mid-2016 and Sydney woman Claudine Fitzgibbon is pregnant for the fourth time when she and her husband Dave start to investigate the possibility of surgery on their unborn son.
They have a three-year-old daughter Eliza and since her birth, the couple has twice made the agonising decision to discontinue pregnancies at about the halfway mark – one in 2014, another the following year. Both babies had spina bifida.
Claudine was induced each time, giving birth to daughters they named Sophie and Willow. The Fitzgibbons were able to hold them and spend a night with them in a special room set up at the Royal Hospital for Women in Sydney.
“It was really quite harrowing,” Claudine says through sobs, the trauma of the terminations still raw.
“There is a certain pressure to feel like you have to make that decision pretty quickly. That’s really hard having a baby that far along and not continuing. It’s a birth. It’s really physically and emotionally incredibly draining.”

When they learned at 16 weeks’ gestation the devastating news their unborn son also had spina bifida, Claudine and Dave were adamant – they could not terminate a third time.
“I really couldn’t fathom losing another baby,” Claudine says.
“The thought of doing that again was just, really, it was too much.”
She turned to her Sydney specialist Dr Antonia Shand and pleaded: “Look, is there anything new? Is there anything different that we can do this time around?”
The timing could not have been better.
Shand was aware a team from Vanderbilt University in Nashville, Tennessee, was preparing to fly into Brisbane to perform Australia’s first in-utero surgery on a spina bifida baby at the Mater Mothers’ Hospital.
The plan was to teach Mater specialists the procedure so they could continue to offer the surgery to couples in Australia and New Zealand.
Shand put the Fitzgibbons in touch with Dr Glenn Gardener, based at the Mater Mothers’ Hospital in South Brisbane.
Claudine and Dave were sitting in their parked car on Queen St, Woollahra, a suburb in Sydney’s east, when they first talked to Gardener about the surgery on speakerphone. They felt a rapport with him from that first conversation.
“He had a really lovely manner, a really easygoing, friendly, down-to-earth nature about him,” Claudine says.
“He answered all our questions, he was very keen, not pushy, but totally keen. All of the right things.”

They flew to Brisbane to talk with Gardener in person. He was honest. There were no guarantees. Prenatal surgery is not recommended in all cases of spina bifida.
Both Claudine and her unborn child would have to pass certain medical criteria for the surgery to proceed, based on research and the experience of overseas centres, which have been performing the operation for years.
“There are a lot of numbers that have to add up, a lot of measurements of the baby,” Claudine says.
“I had to have more scans to make sure everything was what it should be to go ahead.”
Because of the increased chances of a premature delivery after having the procedure, mothers who have had a previous preterm birth are not eligible for the surgery.
Other contraindications include women with a shorter-than-normal cervix and those who have had a placental abruption – when the placenta detaches from the inner-wall of the womb before a baby’s delivery.
Women who opt for in-utero surgery are more likely to require a blood transfusion after the birth and are at higher risk of other complications.
“A study of the procedure in the States demonstrated in some cases, the risk to the mother outweighed the benefits to the baby,” Claudine says.
After being briefed about the pros and cons, the Fitzgibbons flew back to Sydney to mull over their decision.

They left the meeting feeling buoyed, despite having no assurances the treatment would be successful.
“Being given any kind of hope is really helpful,” Claudine says.
“It was in stark contrast, I have to say, to the prognosis we were given for Sophie and Willow.”
As family and friends prayed for them, Claudine and Dave decided to go ahead with the surgery.
They flew to Darwin for a five-day holiday with Eliza before returning to Brisbane for the in-utero procedure in August.
To be successful, the surgery can only be performed within a window of a few weeks. Claudine was 24 weeks’ pregnant when she was wheeled into an operating theatre at the Mater Mothers’ Hospital.
Shand, her Sydney-based maternal foetal medicine specialist and Kate Dyer, the midwife who helped her through the births of Sophie and Willow, flew to Brisbane to watch Gardener and neurosurgeon Dr Martin Wood operate.
“I didn’t know half of what was going on,” Claudine says.
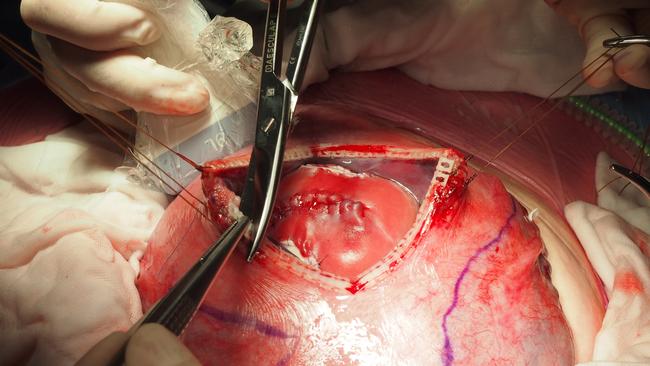
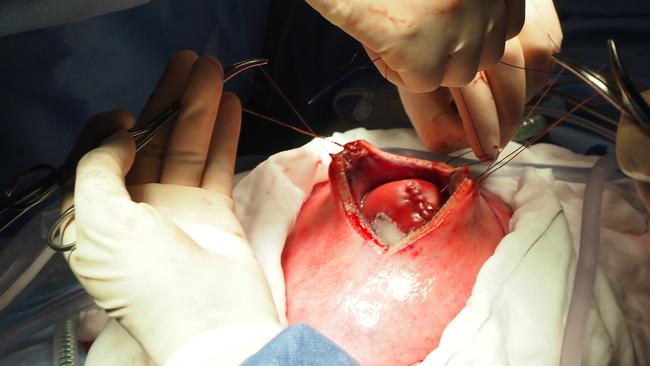
“I spoke to the anaesthetist before the surgery, but it wasn’t until afterwards that I realised the delicate balance of making sure the baby doesn’t get too much anaesthetic while also ensuring the mother is knocked out during the procedure. It was very tricky how much anaesthetic to give because the baby is obviously getting some drugs through the umbilical cord. They opened up my uterus and gave the baby a little needle into his bottom, a painkiller. It’s remarkable. I’ve got all of the photos of the surgery and sometimes I look at them and I just think: ‘Wow’. It’s pretty mind-blowing.”
Claudine spent eight days in hospital post-surgery and then another three weeks with Dave at an apartment near the Mater before flying back to Sydney.
With a natural birth out of the question following the four-hour operation, she was booked in for a planned caesarean at the Royal Hospital for Women at Randwick, in Sydney’s southeast, at 37 weeks.
But when she went to hospital feeling “quite uncomfortable” a month ahead of the scheduled caesarean, and doctors diagnosed low amniotic fluid, they opted to intervene earlier than planned. Harvey George Fitzgibbon was born seven weeks before his due date at midday on October 31, 2016, weighing 2.1kg.
He was taken to the neonatal intensive care unit needing breathing support because of his prematurity, and bore big scars from the in-utero surgery, but otherwise “looked good”, his mother says.
Amid the joys of having their son, those first few days and weeks of his life were also stressful, his parents waiting for signs of the success – or otherwise – of the operation. The anxiety continued after they brought him home on November 25, 2016.
“Always as a little baby, I’d be thinking: Is his back sore?” Claudine recalls.
“We’d say to the doctors: ‘When will he be out of the woods?’ They’d be doing all of these tests and they go on and they go on.”
And then, at 17 months old, Harvey pulled himself up and started walking – well within the normal age range, taking into account his premature birth.
“He hit all his milestones on time,” Claudine says.
“There were no delays. We were fully expecting him to have some sort of difficulties with walking or problems with his bowel or bladder. Never in our wildest dreams did we think he would be totally fine.”
Spina bifida is diagnosed in about one in every 2000 Australian pregnancies, many of them ending in termination.
In babies with the severely disabling condition, the lower part of the spine fails to develop normally, leaving nerves exposed and at risk of damage. Many children with the condition are unable to walk and can have trouble controlling bowel or bladder function.
While surgery in the womb to cover the nerves is not a cure for spina bifida, Gardener says it doubles the chances of a child being able to walk unassisted. It also lowers the risk of the babies being born with fluid on the brain, requiring the insertion of a shunt, which can have lifelong complications. Mater hopes to be able to provide about 10 in-utero surgeries for spina bifida each year in Brisbane.

“The families that we see teach us a lot about resilience, persistence and seeking nothing but the best possible outcome for their child,’’ Gardener says. “Watching these children grow up is really a privilege.’’
Harvey is aged 5 now and a brother to Eliza, 8, and the newest addition to the family Genevieve, 2.
He can ride a bike without training wheels and is a proud member of the Maroubra Saints under-6s AFL team.
“Almost every week when we see Harvey on the football field, Dave and I are like: ‘Gosh, that’s just so remarkable. That’s such a miracle’,’’ Claudine says. “I don’t think I have the words for just how grateful we are.”
You can support life-changing surgery to help children like Harvey through buying tickets in Mater Prize Home. You really are changing lives with every ticket that you buy.
Tickets from $2 at materlotteries.com.au or call 1800 067 066.
iN PARTNERSHIP WITH MATER PRIZE HOME




