The joy of (safe) sex: where Australia really stands with contraception
Let's talk about sex

Lifestyle
Don't miss out on the headlines from Lifestyle. Followed categories will be added to My News.
While rolling condoms on bananas may be a distant sex-ed memory, normalising and continuing conversations about safe sex is incredibly powerful and – as shown by the results of the Body+Soul 2024 Sex Census – also very necessary.
Contraception and protection can be a complex area, influenced by everything from old taboos to convenience and cost. That’s why one important mission of the Body+Soul 2024 Sex Census was to uncover Aussie attitudes to safe sex and reveal how we’re really navigating it in 2024.
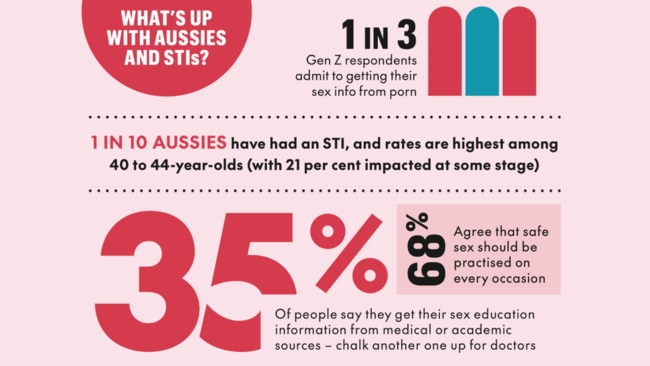
And the results were intriguing, to say the least. While a solid 68 per cent of you agree safe sex should be practised on all occasions, only 15 per cent use contraception every time they have sex and 13 per cent do ‘most times’. What’s more, one in 10 ‘hardly ever’ use protection, while an alarming 26 per cent of Aussies ticked the ‘never’ box.
So what’s driving these choices, and how can you level up your sexual health knowledge? Read on. We’ve got you, well, covered.

Great barrier grief
When it comes to why almost a third of us might swerve contraception altogether, Dr Sara Whitburn, Deputy Medical Director at Sexual Health Victoria, explains there are multiple potential barriers. Think: lack of access, expense (the pill, for example, can set you back up to $30 monthly) and discomfort around broaching the topic, especially if you’re re-entering the dating arena after a long-term relationship or sexual hiatus.
“There can be stigma around trying to have that conversation when you’re out of practise,” she explains. “It can be seen as not ‘sexy’ or ‘fun’, so it’s about supporting people in making that a part of the discussion – not only what you like [sexually], but what you want to use for protection.”
Like overstaying that great park outside your coffee spot, a classic “it won’t happen to me” mindset can also see caution go MIA in the heat of the moment, adds clinical sexologist and relationship counsellor, Naomi Hutchings. “People think ‘it’ll be fine’ and then, if nothing happens, they’ll do it again,” she tells Body+Soul.
Contraception confusion
As for the modus operandi of those respondents who say that they do use contraception, there seems to be some confusion about what actually counts as a barrier method. In our survey, condoms were the most used form of contraception at 68 per cent, with oral forms (aka, the pill) claiming second at 23 per cent.
Other methods that Aussies surveyed said they use as ‘contraception’ include withdrawal (seven per cent) and peeing, showering or cleaning up afterwards (four per cent). And no, we’re not joking.
It’s crucial to recognise here that some of these methods are far more effective than others – both in terms of contraception and preventing the spread of any sexually transmitted infections (STIs).
As the Department of Health wisely explains, “A condom can protect you from catching or spreading an STI and from unintended pregnancy. Even if you’re using a different method of contraception to prevent pregnancy, you still need to use a condom to protect you from STIs.”
And that goes for everyone from TikTok-loving Gen Zs to Boomers who are back on the dating scene after a long absence, with the ‘silver divorce’ trend continuing to grow not just nationwide but around the world.

“The efficacy of the withdrawal method can be as low as 40 per cent,” notes Dr Whitburn about methods of contraception. “It relies on the person with the penis withdrawing at just the right time, and we know there can be sperm in pre-ejaculate, too. Whereas condom [efficacy] can be around 98 per cent with perfect use.”
Turns out that tech is also making an impact. Some three per cent of respondents to our poll said they use fertility awareness-based methods – which involve decoding the fertile points of your menstrual cycle using tools such as apps – as contraception. But the efficacy of this depends on a lot of variables, including cycle regularity and super-consistent tracking, explains Dr Evonne Ong, Medical Director at Family Planning Australia. “Even for people who have very regular periods, many of us have experienced firsthand how stress, dietary changes or poor sleep can cause a disturbance in the cycle – which can then change when you’re ovulating next.”
It also goes without saying that peeing, showering or cleaning up after having sex definitely isn’t a form of contraception, and crucially also won’t protect either partner from STIs.

Testing times
And what about STIs? We’re glad you asked. According to our survey, of those who’ve had one, a fifth didn’t tell any former partners, demonstrating the need for more transparency in this particular sexual health space.
Dr Ong states how important it is to tell former bedmates if you discover you have an STI – “so they can get tested and treated if needed” – also noting that STIs like chlamydia and gonorrhoea can be asymptomatic.
However, while there is still progress to be made when it comes to conversations about sexual wellness, telehealth and online services are offering new pathways to care and advice about both contraception and sexual health. Sites like Let Them Know (letthemknow.org.au), which is a free, anonymous tool for notifying sexual partners that they may be at risk of an STI, have been developed in recent years to help make the whole situation way less awkward.
Another massive leap forward? Everything from dental dams to STI test kits are now available online and are just an ‘add to cart’ away. Melbourne researchers are even trialling free vending machines offering the latter to help make access to these game-changing sexual health tools easier, no matter where you live.

Wrapping it up
Clearly the safe-sex space still has obstacles to overcome, whether that be access and education around contraception, or more open and honest conversations about STIs. However, the dialogue and story sharing around contraception has never been greater, and this is without doubt a step in the right direction.
When it comes to sexual health, the experts advise revisiting your approach to it often – just as you would your other health and wellness regimes. “At every age, it’s thinking about what’s sexually healthy for you now,” says Dr Whitburn. “Where are you in your current life stage? Who are you with? Is it time for a sexual health check? What are your plans? It’s a holistic approach.”
The final word? It’s time to welcome a new age of treating our sexual health like any other aspect of wellbeing. One where we feel empowered to talk about choices – with partners as well as health pros – while stigma and taboos fade into the past.

How to nail sexual health
Upgrade your safe-sex script with these cringe-free strategies from leading experts
#1. First, make safe sex sexy
Bringing up protection – via message or face to face – is a step towards making it a regular part of your dialogue. “You could say, ‘Just so you know, I've had an STI check recently,’ or, ‘I’d like to use condoms – shall I bring them or will you?’” tips Hutchings. “Putting it out there can be scary, but you’re creating an open space to have that discussion.”

#2. Read your partner’s vibe
If your sexual partner tries to shut down conversations about safe sex or convince you to ditch your boundaries, this should be an immediate red flag. “Never apologise for asking someone to be safe,” says Hutchings. It’s non-negotiable in any healthy relationship or hook-up. Safe sex can (and should) be sexy, so treat it like any other form of foreplay.
#3. Put the emphasis on equality
Repeat after us: it takes two to tango. While the scientific quest for new male contraceptives continues, check in with your partner about balancing the load. “Can they pay for your birth control for a few months?” asks Hutchings. “You’re a team, and it’s about sharing responsibility.” And that goes for everything from condoms to lube and open conversations.
Can't get enough? For all the spicy details from our nationwide survey, head to bodyandsoul.com.au/sexcensus
More Coverage
Originally published as The joy of (safe) sex: where Australia really stands with contraception




