Why there is an urgent need to rename Polycystic Ovary Syndrome (PCOS)
It is a serious and common condition but it’s misleading name has caused delays in diagnosis. This is why it’s going to change.
Conditions
Don't miss out on the headlines from Conditions. Followed categories will be added to My News.
A common, but poorly understood condition affecting one in eight Australian women will get a new name after health experts and patients agreed the current one was not only misleading, but causing a delay in diagnosis.
In a major study, 7708 patients and health professionals from six continents were asked about Polycystic Ovary Syndrome (PCOS) and 87 per cent said it needed a new identity.
The study was led by Monash University Professor Helena Teede with the results published on Thursday in the Lancet’s EClinical Medicine.
Professor Teede leads the Monash Centre for Health Research and Implementation and the NHMRC Centre for Research Excellence in Women’s Health in Reproductive Life at Monash University. She is also an endocrinologist at Monash Health.
“The name PCOS does not reflect the broad range of health impacts of this serious condition,” Professor Teede said. “It has significant, broad and profound effects on women and takes a long time to get diagnosed. It is also inadequately treated.”
She said a global community had been involved in discussions about a name change since 2012 with the aim to raise awareness, improve diagnosis and develop better treatment.
Asked to name the leading contenders, she said a survey would canvas preferences with a “winner” expected to be announced by the end of the year.
Professor Teede said it could include keeping the acronym PCOS, but changing what the letters stood for.

“It could also be using a single name like diabetes, like asthma, like endometriosis, which actually links to the condition.”
She said terms like ‘endocrine’ and ‘metabolic’ were also strongly supported.
Professor Teede said groups had taken time to find the right name because they wanted to better understand the condition to avoid getting it wrong again.
“I lead the international PCOS guideline development program and that really has been the thing I am personally most proud of; in this study we have also showed that the guidelines have led to significant improvements in understanding of the broad and significant impact of this condition and the importance of a new name.
She said it also brought people together globally so there was a strong voice from those with the condition “who are frustrated, understandably, thinking their condition is reduced to something that’s happening only to the ovaries”.
Professor Teede said PCOS had also missed out on research funding.
“There are brilliant things happening with endometriosis. We’ve seen fantastic things happen with menopause,” she said. “This has to be next in recognition of really neglected women’s health conditions.”

She said the next step was a new name.
“It will help with greater awareness, research funding, education and improved care and outcomes,” Professor Teede said.
“The focus (now) is on ovarian cysts, which are not true cysts but rather eggs or follicles that have stopped growing, and overlooks the impacts of this multisystem disorder, leading to confusion, missed and delayed diagnosis, and inadequate information provision and care.
“The thing about it is that it’s an endocrine or hormonal condition and that’s the bit that’s not been understood.”
Professor Teede said PCOS was the most common endocrine or hormonal condition in reproductive-aged women, yet its name did not reflect the broad range of health impacts.
She said it also carried risks of higher body weight, diabetes, heart disease, fertility issues and pregnancy complications, endometrial cancer, skin and hair changes including acne and excess facial hair, and psychological features including depression and anxiety that were all exacerbated by related higher weight.
Co-author of the study Dr Mahnaz Bahri Khomami said everyone could help decide the new name through the PCOS new name survey.
Lorna’s story
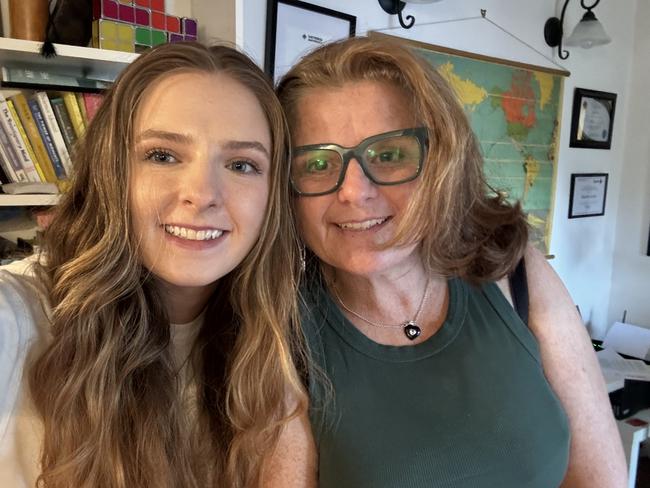
Lorna Berry said it had taken years to get a diagnosis of PCOS. The mum of two is now working with an international team to help rename the condition.
“I think the name is inaccurate,” Ms Berry, 55, said. “It causes all this misconception.”
She said many people confuse it as a disease of the ovaries, because of the name. “And it is not.”
Ms Berry said the aim now was to improve understanding for both GPs and people with PCOS.
“To lead to early intervention and early diagnosis and better outcomes for women with PCOS across their lifetime,” she said.
“This is so important, it is something that affects millions of women.”
She said early intervention was also important for adolescent girls to help prevent weight gain associated with the condition that can also lead to mental health issues
Ms Berry said the PCOS community welcomed the change, which was “a long-overdue shift toward respect, clarity, and meaningful progress”.
Originally published as Why there is an urgent need to rename Polycystic Ovary Syndrome (PCOS)




