Three country psychiatrists not enough. We need at least 10, says deputy coroner in suicide inquest
A young man’s suicide exposes a desperate situation in SA communities, the deputy coroner has warned, and open borders could unleash new stresses.

SA News
Don't miss out on the headlines from SA News. Followed categories will be added to My News.
More than triple the current number of psychiatrists are needed in country South Australia, based on the recommendations of a coronial inquest into the suicide of a 27-year-old Riverland man.
The Deputy Coroner’s call for greater resources comes amid growing mental health concerns for regional communities at the frontline of a new Covid-19 wave expected when the state’s borders reopen on Tuesday.
A peak body says there is “virtually no support for regional staff”, who are overworked in a “completely inadequate” system. It has been lobbying the state government to create localised training and recruitment opportunities.
There are currently three psychiatrists working across Country Health SA’s 13 community mental health teams. They are employed in Berri, Whyalla and Mt Gambier. Two of these positions are temporarily filled.
Deputy State Coroner Anthony Schapel says there should be one full-time psychiatrist employed to work in each of the teams.
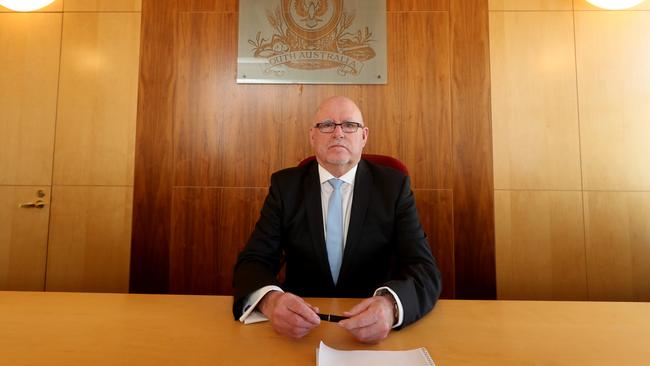
Mr Schapel has directed Health Minister Stephen Wade, chief psychiatrist Dr John Brayley and SA Health chief executive Chris McGowan to conduct a comprehensive review of clinical mental health resources across regional SA.
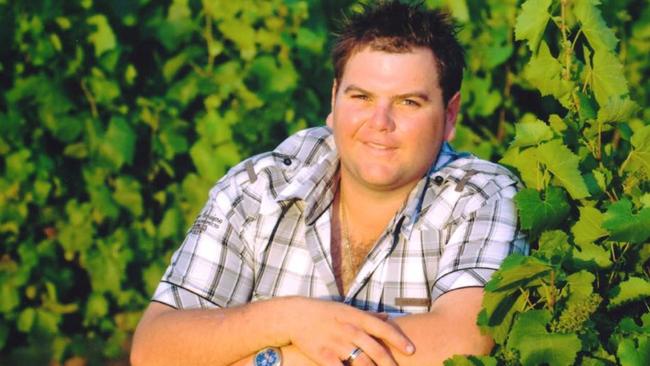
He made the recommendations this month in his inquest report into the suicide death of Theo Nickolas Papageorgiou, from Cooltong, on January 24, 2016.
He died three days before his appointment with the Riverland’s visiting psychiatrist, who last saw him in November 2015.
Associate Professor Mathew Coleman, from the Royal Australian New Zealand College of Psychiatrists (RANZCP), said the inability to recruit and relieve mental health staff from within and beyond SA due to pandemic lockdowns had meant an already lean workforce was on the brink of collapse.
“The few local psychiatrists that exist … are already burnt out and tired and they are now being told to ‘brace yourself because we’re now letting Covid back in’,” said Prof Coleman, the RANZCP’s national chairman of rural psychiatry.
“The impact is greater particularly in SA where you have this metro-centric provision of mental health services to rural SA – it’s completely inadequate – so there is virtually no support for regional staff.”
SA Health’s clinical director of the Rural and Remote Mental Health Service, Dr Brian McKenny, who gave evidence at the inquest, said providing an efficient mental health service for the bush was a challenge due to workforce recruitment.
“There are always vacancies in our community teams,” he said.
He agreed three resident psychiatrists across the whole of SA’s six country health networks was not enough.
Dr McKenny said telehealth had eased some of the strain.
SA Health said it was reviewing the Deputy Coroner’s findings.





