New technologies are accelerating our scientific understanding of cancer and how to cure it
Cancer research and treatment is changing with personalised medicine, computer modelling and 3D printing. These are the latest developments, which will be unveiled at UniSA this week.
SA News
Don't miss out on the headlines from SA News. Followed categories will be added to My News.
Science is increasingly guiding clinicians on how best to treat individual cancers and reduce side effects.
Adelaide research is at the forefront of developments that offer new ways to test drugs, radiation and other therapies outside of the body.
As UniSA medical radiation expert Eva Bezak explains, there are as many different cancers as there are cell types in the body.
And individual patients respond in different ways.
“There will never be one treatment that will cure all cancer,” Professor Bezak says.
“That’s because different cells have different functions in the body, whether it’s blood cells or muscle cells or brain cells, they all have different properties and behaviours.
“Therefore the cancers will behave differently and we have to identify therapy that will affect those particular cells.”

Scientists traditionally develop new therapies in the laboratory, outside of the body in test tubes, flasks and Petri dishes (in vitro) and then take the more promising candidates into experiments in a living organism (in vivo), first in animals then humans.
Computers now offer another avenue for research “in silico”, which alludes to the use of silicon computer chips.
“With the computational power and the information that we have, we can now do lots of research in simulation,” Prof Bezak says.
“If you can do an early triage of what will work and not work, you can potentially save lots of time and money and effort, not to progress certain prescriptions or treatment deliveries to clinical trials.”
She has validated the predictive power of her computational model of radiation therapy for head and neck cancer against 11 international clinical trials.
The model predicted the outcome of one trial that should never have been allowed to proceed and had to be aborted because of severe side effects.
Radiation therapy can damage healthy tissue leading to scarring and other serious problems, but some people are more sensitive than others based on their genetic makeup.
Prof Bezak is working with the Peter MacCallum Cancer Centre in Melbourne on testing a patient’s response to radiation before they are exposed and damage is done.
“If we could do an early test of a patient, by doing a blood assay and hair sample assay, we could determine individual sensitivity,” she says.
“Then you can definitely adjust the treatment regimen, based on their individual sensitivity. That would definitely allow us to deliver much more personalised medicine that would help that particular person have the best outcome with minimal side effects.”

The organiser of Friday’s International Symposium on Bioengineered Cancer Models is UniSA bio-engineering expert Professor Benjamin Thierry.
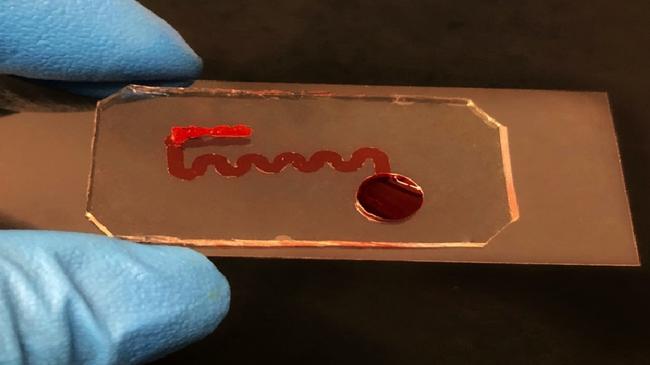
He says technology such as microfluidics and 3D printing offer new ways to test therapy outside of the body that are closer to real life.
“Instead of having cells sitting in a petri dish, now you can grow cells in some sort of small 3D system, where the cells are exposed to the flow of media (liquid containing nutrients, like blood). You can have different compartments with different types of cells and different tissues. These are tools that we are using to recapitulate the complexity of the real tissue.”
After all, he says, real tissue never contained just one type of cell and cancerous tissue contains both the tumour and the healthy tissue of different cell types and structures.
“They usually are exposed to some sort of mechanical stimulation, from the flow of blood,” he says.
“So the tools that we are using allow us to recreate some of they key elements of the physiology.”
In the short term these more complex models are helping scientists to develop better cancer treatments.
He has been looking at the effect of radiation on tiny blood vessels to determine their level of sensitivity.
The cells that comprise blood vessels turned out to be more sensitive when grown on a petri dish than in 3D.
The director of the Dame Roma Mitchell Cancer Research Laboratory, University of Adelaide Professor Wayne Tilley, is developing better preclinical models for two common hormone-dependent cancers, breast and prostate cancer.
His “explant cultures” of human cancer tissues from patients are growing on tiny sponges.
“We tried a completely different approach and partly to our surprise and good fortune, it seemed to work,” he says.
“The tumours for a week or two will grow and sometimes longer, which is ample time for us to apply a whole range of potential new therapeutic drugs and the like.”
The research gives extra confidence that a particular therapy is worth taking through to clinical trials, but there is potential for the same approach to guide treatment of individual patients.
Adelaide company Carina Biotech is also looking at the potential for bio-engineering to guide the development of their promising cancer immunotherapy.
CAR-T (chimeric antigen receptor T cell) therapy is a revolutionary new treatment that uses a patient’s immune system to fight their cancer.



