National Disability Insurance Scheme gap could see a ‘tsunami’ of mental health demand
MENTAL Health Coalition boss Geoff Harris predicts a “tsunami” of demand for services as people miss out on places in the National Disability Insurance Scheme.
SA News
Don't miss out on the headlines from SA News. Followed categories will be added to My News.
- $72 million partnership to deliver frontline help
- Disability advocates worried about a messy move to the NDIS
- Significant mental health issues among firefighters
- Editorial: The challenge of rural mental health
SOUTH Australia faces a “tsunami” of unfunded demand for mental health services because the National Disability Insurance Scheme fails to cover all those now receiving help, advocates say.
The warning comes ahead of today’s forum on mental health where political candidates will reveal their plans for the sector in the lead up to the state election.
Mental Health Minister Peter Malinauskas and representatives from the Liberals, Greens, Dignity and Australian Conservatives have confirmed they will attend and SA Best may have a candidate.
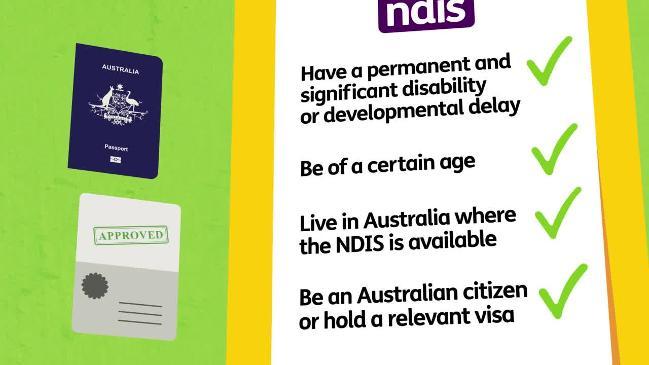
The NDIS – a lifelong insurance scheme providing individual care plans – will be rolled out from July 1 to eligible adults with primary disability from mental illness.

To meet its requirements, a person has to provide evidence they have a mental illness which reduces their psychosocial functional capacity and will require some support under the NDIS for life.
Mental Health Coalition SA director Geoff Harris said 2985 people participated in SA-funded mental health support programs in 2016 but he estimates only 20 per cent would be eligible for NDIS support.
This is because they may have a relatively short term mental illness issue so would not meet the criteria of having sufficiently reduced capacity, including capacity to work, to require lifelong support.
He said the State Government had not indicated what level of support would remain for state programs.

In addition, there were 4012 South Australians participating in Commonwealth funded programs in 2016 but funding for these will cease as NDIS rolls out and the MHCSA estimates about 3045 of these people also are unlikely to qualify for NDIS support.
“What our figures show is that only a small percentage of people are getting in to NDIS and we are facing massive cuts in funding and capacity from July 1,” Mr Harris said. “We’ve been saying for four years the NDIS was no substitute for mental health services. We predicted this tsunami ... we are now seeing unfolding.
“If the State Government – this one or the next – do not listen, we will see a mental health crisis like never before.
“The NDIS is designed to complement the existing mental health system, not replace it.
“However, what we’re seeing with the current funding is an idea that it will eventually replace current community based mental health models.”
Mr Harris called on the State Government to keep funding services to help cover an unfolding gap.
He also predicted an exodus of experienced health workers, saying the switch to NDIS would mean lower pay rates.
“During the transition to NDIS, we need to ensure people who are eligible actually start receiving support before turning off the tap,” he said.
The forum will be broadcast via the MHCSA Facebook page.
BATTLING BIG BUSH SHORTAGE
A DISTURBING gap in help for sufferers of depression and anxiety is emerging, with only three psychiatrists based in rural South Australia compared to more than 200 in Adelaide.
One of the state’s most comprehensive surveys of rural health reveals a growing disparity between country and city mental health services and shows an increase in suicide rates and drug use.
Early findings from the University of South Australia survey were backed by Mental Health Commissioner Chris Burns, whose own research in the past year showed “a clear lack of mental health services in the country that is compounded by the stigma of walking into a mental health clinic”.
Mr Burns said 30 per cent of deaths nationally for 15 to 24-year-olds were the result of suicide. Car accidents were the second largest killer — but even then many of the single-occupant crashes were linked to possible self-harm.

“The linkage between substance abuse, mental health and suicide, it’s tragic,” Mr Burns said.
“There’s also a lot of drug abuse in the Riverland and Mount Gambier area. It’s ice, the people using it are transient and moving from town to town, there’s a lot of homelessness and mental health is very strongly linked to substance abuse.”
Dr Matthew Leach, who is jointly conducting the health survey from the University of South Australia’s Rural Health Department, said that of the 1600 responses so far, mental health and cardiovascular disease emerged as the two major problems facing country SA.
“What it’s suggesting is there seems to be a high level of need around mental health, especially around depression,” Dr Leach said.
Presently, Whyalla, Berri, and Mount Gambier each has only one psychiatrist, with towns forced to depend on fly-in, fly-out support every three weeks. Mr Burns and Dr Leach said more services were vital to these regions.

Dr Leach and Associate Professor Martin Jones, who is also overseeing the survey, this week will target another 160,000 homes across country SA to continue to gauge gaps in rural health services so they could form a blueprint for future planning.
Dr Leach said there was further anecdotal evidence the drug ice shapes as a linked problem with mental health, with Jamestown medics listing it as a key problem.
The mental health issues gripping country regions comes as no surprise to Rural Business Support’s chief executive Brett Smith.
He believed it was well recognised farmers in particular lived in a “risky environment and there’s a lot of pressure on farmers and farming families”.
Commodity prices, rainfall, fires or floods all risked the future of their farms, and Mr Smith said “anyone who has endured a drought would probably be diagnosed with minor forms of depression”.

FARMING GROUP’S SHOW OF SUPPORT
DAIRY farmers battered by a dramatic downturn in milk prices about 18 months ago are struggling with their emotional reserves, according to industry chief Andrew Curtis.
Mr Curtis says the fall in prices when the nation’s largest milk processor Murray Goulburn decided to pay farmers lower than production costs took its toll. “People have battled through that, their emotional reserves are really low and the industry hasn’t bounced back so there are a lot of pressures, we are seeing people who have soldiered on through the dark times who are finding it really tough at the moment,” the Dairy SA chief executive said.
The industry group employs former Mundulla farmer Rick Hinge as Wellbeing Coordinator to support and chat with dairy farmers.
“Community and government support has dissipated but they still get the big bills ... the emotional battery is spent.”

FOGDEN LEADS CHARGE ON MENTAL HEALTH HELP
LAWN bowlers may traditionally be seen as the slow movers in sport but the state’s army of oldies is leading the pack in tackling the blight of mental illness and suicide in our country towns.
Some “17,000 oldies in white on a Saturday” and another 38,000 night owls now have their first mental health ambassador along with a statewide plan to recreate a sense of community spirit.
“Our facilities tend to become a hub in rural communities, you get a lot of farmers, and mental health and suicide, we’re not immune to that,” Bowls SA chief executive Mark Easton said.
“Certainly every club would be affected by suicide, particularly in the rural space where some farmers may be losing family farms … but I don’t think any sport would be immune.”
It’s an issue that drew the state’s bowlers together to brainstorm ideas and late last year they shared their plans to support families with the state’s Mental Health Commissioner Chris Burns.

“I think we have a role to play, in bowls we have a very inclusive nature to it, we don’t discriminate on any grounds,” Mr Easton said, adding that clubs wanted to also support those who were lonely.
“It’s one of the only sports where you can gather people in and walk up and down and have a chat and do some networking.”
Mr Easton believes there’s a golden opportunity for bowlers to host events at their 220 venues around the state and to help rebuild neighbourhood networks eroded by television, screens and crumbling numbers in church congregations.
Former Loxton lad, footy player and reality TV show House Rules star Brooke Fogden has stepped up as the sport’s first mental health ambassador after getting involved with reviving the now thriving Millswood Bowls Club in Adelaide.
“I think everyone has struggles in different ways,” Mr Fogden said.
If you or someone you know needs help, contact:
LIFELINE 13 11 14
BEYONDBLUE 1300 22 4636
MENSLINE 1300 78 99 78


