Barossa Valley announced for pilot plan to bridge mental health gap
The Barossa Valley would be the site of a collaborative effort between GPs and service providers to help mental health patients waiting for specialist help.

SA News
Don't miss out on the headlines from SA News. Followed categories will be added to My News.
Mental health services are one of the great city-country health divides, but an innovative plan hopes to help bridge the gap as “the glue keeping people together” while waiting for a specialist appointment.
The Mental Health Coalition of SA (MHCSA) is proposing a pilot plan where mental health peer support workers would be based in GPs practices to work with patients seeking mental health support.
After a GP assessment and creation of a mental health plan, the support worker would help the patient determine the challenges impacting on their mental health, develop a plan to assist them and connect them to services in the area.
It would work alongside clinical support and “be the glue that holds people together” while waiting for a psychologist or psychiatrist appointment.

MHCSA executive director Geoff Harris said investing in psychosocial support, such as support workers Kerry McWaters and Daniel Larsen from Centacare is far cheaper than continuing to invest in hospital based services.
“Psychosocial supports are proven to reduce the number and duration of crises by helping people work through difficult problems that are also impacting on their mental health,” he said.
“It will have a big impact on unnecessary admissions to hospitals. This reduces pressure on emergency departments and acute care services as people are supported to be more well, more of the time.
“They are services that help people manage day-to-day when they are in a mental health crisis – or feel one coming on.
“They work alongside clinical support like psychologists and psychiatrists and are a kind of glue that keeps people together between appointments. The way they support people is by helping them with employment, housing, and everyday tasks that can cause stress and impact on a person’s mental health.”
MHCSA sought out a network of GPs and services in the Barossa Valley where there are already collaboration between groups of mental health and community stakeholders, and says the proposed pilot would cost $1.86m a year.
It comes against the backdrop of the Chief Psychiatrist’s Unmet Needs Study which estimates some 19,000 people with severe mental illnesses are not getting the services they need and an estimated $125m a year is required to fix the shortfall.
Tanunda GP Bill Gransbury said there are long waits for specialist support outside Adelaide.
“In order for it to work, the patient will need to attend a practice,” he said. “Some towns do not have GPs. Those that do have GPs do not have bulk billing, so that will be a
barrier for people with severe mental illness.
“We also have social determinants of health driving social issues such as affordable housing, transport, money for food, less social connections post Covid and isolation which add to mental distress.
“We are making referrals to services they need — but the service doesn’t exist, for example there is a lack of emergency housing in crisis situations for people experiencing domestic violence.”
He stressed collaboration between service providers was crucial for good outcomes.
City refuge during toughest time

Robert Clayson now has made five trips from Mount Gambier for cancer treatment, with all the stress, costs, work absence and other disruptions extended trips from home entail.
His story is typical of the city-country divide when it comes to some specialist care — country residents have to head to Adelaide.
Mr Clayson, 53, has had regular blood tests since turning 50 and his GP did not like the direction of his last PSA count so referred him to an Adelaide specialist who on May 31 diagnosed prostate cancer.
Scans showed he also had thyroid cancer, and on July 5 his thyroid gland was removed in Flinders Private Hospital.
“There was a 3cm tumour on the thyroid and it was on the move, so I am lucky they picked it up when they did,” Mr Clayson said.
On August 7 he was back in Adelaide yet again to have his prostate removed, this time at Ashford Private Hospital.
“I’m glad I had private health cover as I wanted it done as soon as possible — I still had to pay a bit but that’s how it rolls,” he said.
Mr Clayson, who works for Caterpillar dealer Cavpower, has stayed at Cancer Council SA’s Greenhill Lodge while having treatment and is full of praise for the 140-room supported accommodation facility for country cancer patients.
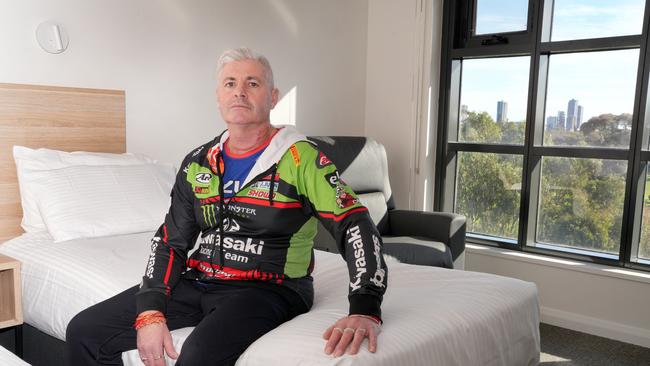
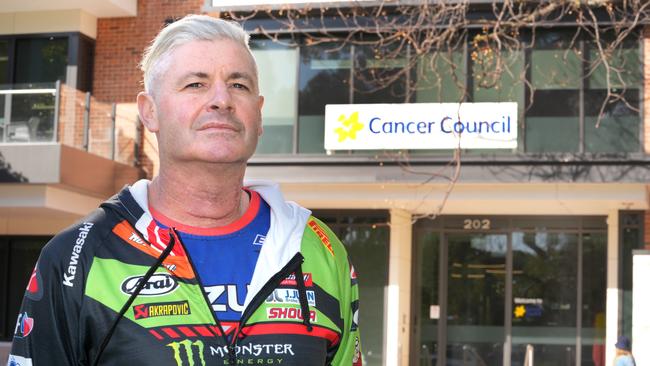
“It really is a home away from home, there are so many other things to worry about and this is just a great escape, you can cook and wash and I have met plenty of other people from Mt Gambier and other regions.
“If you have to come from the country you worry about the cost, about having someone look after your place, being away from work, it is pretty hard.
“Mt Gambier and district is home to about 25,000 to 30,000 people but you still can’t get some medical services there, and now plans for a local radiation therapy service are not going ahead.”
An independent report for SA Health released last month found establishing a radiation therapy service in the region, using a fly-in, fly-out specialists, is “not a safe, sustainable, or financially viable option.”
Local authorities are pursuing other support for patients including advocating for “adequate compensation” for travel.
Cancer Council SA is working to reduce the impact of cancer for all South Australian, noting almost one in two people will be diagnosed with cancer by the age of 85.
“As South Australia’s leading cancer charity, working across every aspect of every cancer, we are committed to helping any South Australian facing a cancer diagnosis, regardless of where they live,” a statement says.
“We welcome regional guests at our Lodge as a home-away-from-home while they have treatments and cancer related appointments. We offer the most up to date accommodation alongside on-site support services including social workers and transport to treatment, kitchen and dining areas and welcoming communal spaces.”
Cancer Council SA has 131120 telephone information, support and counselling services. It relies entirely on donations, and has Daffodil Day on August 22 as a major fundraiser.





