South East advocate concerned about cross border communities accessing voluntary assisted dying
With new VAD laws due to come into force in South Australia, advocates are warning some terminally ill patients could be cut off.
Mount Gambier
Don't miss out on the headlines from Mount Gambier. Followed categories will be added to My News.
A South East voluntary assisted dying advocate has called for clarity ahead of the January 31 commencement date of new laws that empower those with a terminal illness to end their own life.
Jane Qualmann, a former nun who is also suffering from a terminal illness, has been a staunch proponent and welcomed the legislative change.
However, she expressed concern patients in regional areas would face additional barriers in accessing the service.
Compared to Queensland, which has over 300 doctors trained to assess VAD patients, Ms Qualmann said 42 doctors across SA was a disappointing figure.
“I know there is a doctor shortage and I respect that,” she said.
“(But) there’s only five navigators in SA, with one rural and remote care navigator.”

Ms Qualmann said accessing a doctor who did not consciously object was going to be incredibly difficult and would almost definitely mean travel for rural patients.
Voluntary Assisted Dying Implementation Taskforce chair Dr Chris Moy acknowledged regional patients faced some barriers but said there was “nothing stopping some of the assessment being done via telehealth”.
Ms Qualmann said more information needed to be available, given that doctors are expressly forbidden from discussing or even mentioning VAD with their patients, unless the patient themselves brings the topic up.
“People still don't know what VAD is — I just wish that it was simpler for people to navigate through the website,” she said.
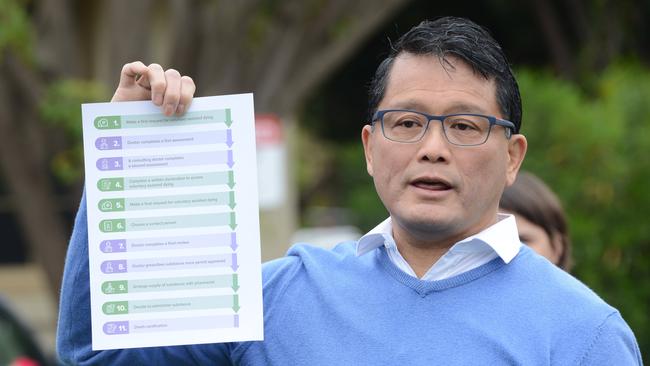
There are strict measures in place to ensure VAD patients come to the decision without coercion.
Dr Moy said there was still a lot of misunderstanding around VAD and what it means for palliative care options.

Dr Moy said palliative care manages a person’s symptoms until their death, whereas patients who choose voluntary assisted dying actively take medication to end their life.
“Palliative care, which has been the bedrock of end-of-life care, is still going to exist and still going to be the main foundation of end-of-life care,” he said.
“I hope families can have mature discussions among themselves. It is reasonable to bring this up as an option within family — (but) health practitioners can’t bring this up as an option at all.”
Dr Moy warned coercion might not just be statements such as “you should”, but included “continuously repeating it as an option” or attempting to guilt someone into taking VAD as an option.
Ms Qualmann said terminally-ill patients should be given an end of life package — with pamphlets, factsheets and information on all their options, including voluntary assisted dying, to both inform patients and avoid pressuring them either way.
Allaying concerns raised by residents from cross border communities, Dr Moy said “you would not need to start from scratch” with evidence from interstate doctors and specialists allowed for the initial diagnosis and assessment.
“A patient seeing an oncologist in Victoria would not have to see another oncologist in Adelaide just to confirm the diagnosis,” he said.
However, both the coordinating and consulting doctor needed to conduct their assessment from South Australia.
“A doctor from Victoria could provide VAD in SA as a co-ordinating or consulting doctor as long as they are in the state while carrying out all the VAD activities specified under the Act,” he said.
Interstate doctors will also need have carried out the mandatory South Australian training and be registered in SA to provide VAD.





