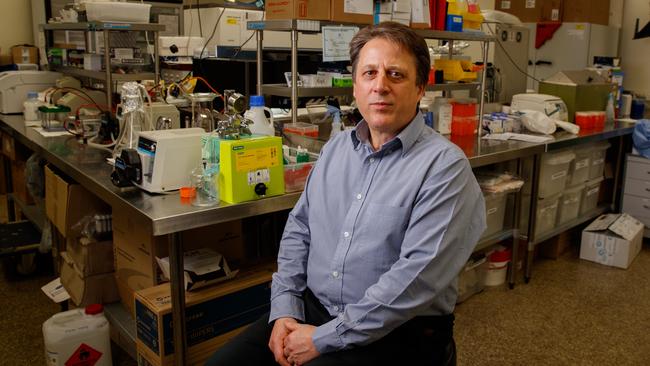
COVID vaccine: SA scientist Nikolai Petrovsky to launch a world trial of his Covax-19 vaccine
An Adelaide COVID-19 vaccine is set to be the first from Australia to make international trials, with or without federal government backing, says developer Nikolai Petrovsky.
SA Weekend
Don't miss out on the headlines from SA Weekend. Followed categories will be added to My News.
- Wildlife wars: Avoiding the next pandemic
- How cricket saved an Afghan war survivor
- Feeling smart today? Take the Brainwaves quiz
Nikolai Petrovsky has little time for socialising right now, but he’s grateful he once did. If the Flinders University professor can produce an effective COVID-19 vaccine to help save the planet, it will all come back to a conversation over drinks in Canberra one night in the early 2000s.
In July, Petrovsky’s Covax-19 became the first Australian vaccine to be tested on people. While results haven’t been officially completed, he says this small Phase 1 trial showed the vaccine was safe, well-tolerated and stimulated an immune response.
Given vaccine testing can make disease worse or people sick, those are magic words. Now Petrovsky plans to go the Full Monty with a large international trial which he hopes will include elderly residents of Melbourne aged care homes, who are at highest risk of dying from the virus.
This combined Phase 2/3 trial, involving 20,000 or more people in countries rife with COVID-19, will be the acid test as to whether his vaccine can stop the infection that has already killed more than 800,000 people worldwide.
At this stage, and his plans are constantly changing as he seeks backers, the aim is for the trial to take place in October and November, potentially determining by the end of the year if the vaccine is effective.
Nobody – including the scientists behind the Oxford vaccine Australia has signed up for, or any of the other 40-odd vaccines now in human trials – really knows if their product works until after this crucial phase is completed.
There are some caveats. Petrovsky’s company, Vaxine, hasn’t yet got the many millions of dollars, or a solid deal with a major pharmaceutical company, usually needed to pay for a Phase 3.
Also, he says, it has struggled to get the attention of the Morrison government, which has put millions into a competing University of Queensland vaccine project.
But Petrovsky, who has received tens of millions of dollars for pandemic vaccine research from the US government over the past 15 years, is undeterred.
He is hopeful of Australian support but says he’ll keep going regardless, and sounds confident that he will be in a position to find an ally – whether a company or a country – to put his vaccine to the ultimate test.
“We won’t give up,” he insists, in his office at Flinders Medical Centre. “We’re looking at novel ways to develop a billion-dollar vaccine, without actually having a billion dollars.”
But first, that drinks party in Canberra, because none of this would be happening if the endocrinologist – a specialist in hormones, the body’s molecular messengers – hadn’t got chatting with retired biochemist, Dr Peter Cooper.
Petrovsky, 61, grew up in Launceston. His father, a tropical medicine expert and ex-prisoner of the Japanese on the Burma railway, ran the hospital, and his mother was a GP. He studied medicine at the University of Tasmania and by the early 2000s was working at the Canberra Hospital.
Petrovsky had completed a PhD on development of a type 1 diabetes vaccine by then and was keen to continue vaccine research.
And then one night he met Cooper, a scientist who had trained in London with Alexander Fleming. Fleming, with Adelaide’s Howard Florey, won the Nobel prize for discovering penicillin.
Cooper had returned to Australia to work at the Australian National University on a cure for cancer. In the course of his research, he’d discovered a plant sugar-based compound called gamma inulin, which he showed was effective against cancers in animals, but which he had never succeeded in having tested in the clinic.
Still, Cooper had pressed on. “He investigated what else the plant sugar might do and generated some data before he retired suggesting it had an effect on the immune system,” Petrovsky recalls.
“That was the theory as to how it was working as an anti-cancer compound. It sounded like an intriguing story. I didn’t quite believe it. It sounded a bit too good to be true.”
But scientific advances are often thanks to serendipity, he says. “Given I had a lab and because I wasn’t grant funded, I was able to work on anything I liked, so I said, ‘Drop some off if you’ve got some’. He said ‘I will have a look but I am sure I’ve still got some samples lying around somewhere’.”
Cooper’s discovery didn’t help the diabetes vaccine Petrovsky was working on, but he had other vaccines, like hepatitis B and tetanus, so he tried it on them.
This time the results were very good, just as Cooper had predicted. What he had was a very effective adjuvant, something that acts like a turbocharger for vaccines.
And then President George W. Bush stepped in. Shortly after the strikes of September 11, 2001, the US was hit by a biological warfare attack via the mail system, using anthrax, a deadly bacterium that the US no longer had vaccines to counter.
Bush threw billions of dollars at rebuilding the US’s vaccine-making capabilities, a drive boosted when Severe Acute Respiratory Syndrome (SARS), caused by a coronavirus, broke out from China in 2003.
Once again Petrovsky hit the jackpot. The US National Institutes of Health, which controlled Bush’s vaccine research money, put out a call for proposals – and somehow, he heard about it.
“We assembled a proposal around the sugar compound from Peter Cooper and our data, and said we think this could be applied to SARS and anthrax vaccines and all
the other organisms like Japanese encephalitis they were putting as high biodefence priorities,” he says. “And I thought it had zero chance of success based on the outcome of my Australian grant attempts – but what did I have to lose?”


This was American money, after all, and likely to all be given to American researchers. And for two years it looked like he was right – until one day in 2004, as he was about to move from the Canberra Hospital to a new position as Director of the Endocrinology Department at Flinders Medical Centre, an email popped up.
In a brief message, the NIH told him it had just awarded him a $US2.5 million grant for his vaccine development. In Australia, he’d have been lucky to get $250,000 for three years of research, and here was the equivalent of about $A4m over five years.
Petrovsky was stunned. There were minimal instructions, in effect “please send us you account details so the funds can start to be paid”.
“I didn’t believe it after two years of complete silence and thought it was a scam,” he admits. He emailed back to be sure they’d got the right people. Then he jumped on a plane to Washington to meet NIH staff who blamed national security sensitivities and paperwork errors for the delay.
Since then Vaxine, the company he set up in 2002, has received about $A50m from the NIH for work on multiple vaccines – including SARS and MERS coronaviruses, swine flu and bird flu – and the use of artificial intelligence in vaccine design.
The reason Petrovsky is confident about his new vaccine is the work he’d already done on SARS, a coronavirus with a spike protein genetically very similar to the COVID-19 virus.
A VACCINE MIGHT HELP ONLY HALF WHO GET IT
One of Vaxine’s first projects was to apply its adjuvant technology to US-made SARS vaccines that were making the animals on which they were tested sicker when they were exposed to the SARS virus than non-immunised animals.
“That is the worst possible outcome when a vaccine actually makes the infection worse,” he says. “They halted the advancement of those original SARS vaccines into humans because of the safety issue. They (the NIH) asked, can your adjuvant fix it?”
The NIH funded the University of Utah to test the SARS vaccines with Vaxine’s sugar-based turbocharger and, Petrovsky says, “we got complete protection against the virus and also against the vaccine-enhanced disease”.
Had that gone through to successful human trials it would have been the world’s first coronavirus vaccine. But despite its promise, the SARS work made it no further. The disease died out from the human population, and others like ebola raised their scary heads. Funding disappeared.
How confident is he that the vaccine would have worked in people? “You can’t assume that what works in animals, works with humans,” he says. “But if it doesn’t work in animals, it’s almost certainly not going to work in humans.”
The tragedy of the halt on all the SARS work was that success would have put scientists in a much stronger position to deal with COVID-19, the disease caused by the SARS-CoV-2 virus. Petrovsky says he warned that a coronavirus could return to cause a new pandemic.
But at least the SARS work has provided the basis for his new vaccine. “We knew the spike protein approach worked and it’s the identical approach we’ve taken to COVID,” he says. “It’s the same platform, the same sugar-based turbocharger. With SARS the spike protein is 85 per cent genetically identical to COVID, so very similar.”
Petrovsky’s vaccine is one of a Melbourne Cup field. There are about 180 vaccines in development against COVID around the world, and his Covax-19 was the 16th of about 40-odd now in human trials. The University of Queensland vaccine has now also entered human trials.
Russia claims to have a working one, as does China, but in terms of a vaccine that has gone through the full set of rigorous human testing, there is none.
One of the early candidates is the vaccine developed by Oxford University and British-Swedish company AstraZeneca, now in Phase 3 trials, which could be available later this year or early 2021. Earlier data showed that vaccine triggered an immune response although a significant proportion of participants had fevers and flu-like symptoms.
The Morrison Government says it has arrangements in place – although the details are unclear – to purchase sufficient doses for Australians if the vaccine works.
But even if it does, it may not be the best option. Vaccines vary widely in their effectiveness. A later one could be much, much better. So, what is a successful COVID-19 vaccine? The World Health Organisation and the US Food & Drug Administration say 50 per cent effectiveness is the minimum.
That’s the level of flu vaccines, which may protect only half of those immunised, and well below something like measles, which is in the high 90 per cent range, and can bring herd immunity.
Fifty per cent would save many lives, especially if it worked well among the elderly – but experts say it would not stop the pandemic or end social distancing. They say it would need to be at least 80 per cent and preferably higher to do that.
And even if it were a very effective vaccine, say 90 per cent, it might not be rolled out worldwide quickly. Petrovsky says it could take years to make and deliver at least 7.5 billion shots for the entire planet, double that if two doses are needed for each person. It might also need annual boosters.
All that, he adds, makes it likely multiple vaccines will be needed. Which makes him even more frustrated that while the US has poured billions into its Operation Warp Speed vaccine program, Australia has not had the same sense of urgency to fund vaccine projects – including his.
VACCINES WORK “LIKE AN EARLY WARNING SYSTEM”
Some experts, like infectious diseases specialist Dr Paul Griffin from the University of Queensland, say Petrovsky will win Australian support if his data is good. Griffin welcomed the news that Vaxine’s product completed Phase 1, but says the numbers – 40 people – were small and peer-reviewed details are yet to be released.
“We need to be evidence-based and so all claims need to be well-substantiated,” says Griffin, medical director of Nucleus Network, experts in Phase 1 trials. “I would be very confident if there was robust data that said it was as successful as he’s suggested in media releases, he should very easily be able to obtain the funding that he needs.”
Petrovsky says the results should be completed any day. But he says his track record deserves credit, given that Vaxine has taken four pandemic vaccines into human trials, while the University of Queensland had never previously done any such trials.
While he concedes none of his vaccines has yet hit the market, he says the usual development period is 15 years, so that is no reflection on the quality of his science.
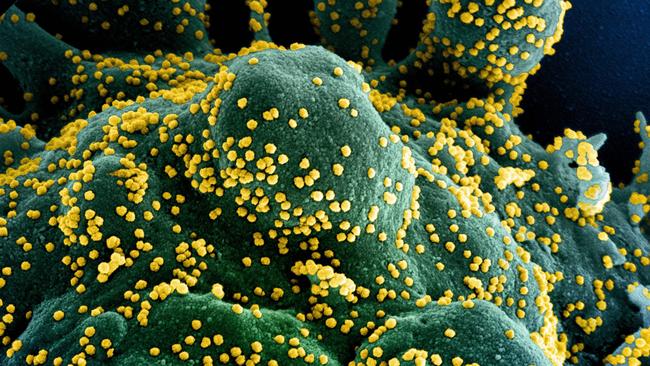
So how does Petrovsky’s Covax-19 vaccine work? First, he says, you need to understand how a virus infects the body. A virus is a microscopic parasite that can’t thrive by itself. It needs to get inside our cells, hijack the machinery that makes our genetic material, and start replicating itself.
The COVID virus is like a sticky ball. In this case, the sticky bits are its spikes, which bind to a protein on the surface of many human cells called the ACE2 receptor. Like a key in a lock, it opens the cell, allowing the virus to enter and start replicating.
Our immune system counters such bugs in two ways. The innate system activates within minutes of an infection, launching an indiscriminate counter-attack – heating the body, slowing the cell machinery that viruses need to hijack. It’s a shotgun approach designed to make any bug uncomfortable, and it makes us feel terrible.
“That buys time,” Petrovsky says.
The second part is the adaptive system, with B cells and T cells. The B cells make antibodies, whose job is to lock onto a specific virus, stop it from infecting cells and help kill it. Enough of those and the virus will never infect us.
The T cells’ role is the second line of defence, where our cell has been infected and turned into a virus factory. The antibodies can’t go in there, so the only option is for the T cells to kill our own infected cells.
Vaccines act like an early warning system. Those B cell antibodies need to know what the virus looks like, in order to create the shape that can lock on. If the body has never seen that virus before, it risks being overwhelmed before it can fight back.
The vaccine aims to show the immune system in advance what it should be looking for – in this case the spike protein of the coronavirus – and memory cells lock in the information for any future attack.
Vaccines try to achieve this in different ways. The Oxford/AstraZeneca model uses a monkey virus to carry those spike proteins into human cells, triggering the immune response and priming the body for COVID-19.
SA NEEDS TO BE HEARD IN CANBERRA
Petrovsky’s vaccine is different. Vaxine, like the University of Queensland’s immuniser, doesn’t use a real virus but synthetic proteins that mimic the coronavirus spike, which, with adjuvant “turbochargers”, create an immune response.
“Every antibody recognises a different shape,” Petrovsky says. “If we can teach the immune system to recognise just that spike protein, then if they see it on a virus, they will lock onto it so it can’t stick to the cells and get inside.”
Petrovsky’s plans for combined Phase2/3 testing rely on money. It’s enormously expensive to immunise so many people.
Normally a big pharmaceutical company would be needed – or a national government – in exchange for access to the vaccine. Either, he says, are possible.
If not, he hopes to be included in a World Health Organisation Phase 3 trial of multiple vaccines. Even if WHO agree, Petrovsky would have to provide maybe 40,000 doses of a vaccine, which could cost millions. He says he’s in talks to do just that.
Private donors have helped. Earlier in the year he was given $200,000 from US philanthropic source Fast Grants, which raised cash from entrepreneurs like Elon Musk.
Perhaps his willingness to criticise Canberra for his lack of funding – he’s been on Sunrise, Four Corners and in most newspapers – has not helped? “I don’t think it’s in Australia’s interests for vaccine developers to be quiet, and University of Queensland, in particular, has been very vocal,” he says. “So it is important for us in South Australia to be heard in Canberra.”
Besides, he thinks there is likely to be more than one winner in this. Many vaccines are using untried techniques. If his more conventional vaccine is effective, and the radical approaches fail, he thinks the big pharma firms will want to back him.
“It may be if we are right, and protein (vaccines) give the highest level of protection, that the others will fall by the wayside,” he says. “Then what I would expect to see is everyone who had committed billions to their virus vaccines would jump in and start making the protein vaccines.
“If someone fails with their original approach, but they have lots of money and set themselves up to make lots of vaccine, and another category is successful, the obvious thing to do is for them to partner with someone like us who is doing the protein approach.”
So while it’s a big field, there can be multiple winners. “If a horse falls over, the jockey can get on another one and keep going. Say AstraZeneca’s (Oxford) virus vaccine isn’t crash hot – they have got the capacity to make billions of doses, why wouldn’t they just then come and partner with us?”
That would assume that Petrovsky’s vaccine works. He is optimistic. “If we just keep moving forward, as long as our data is strong, we’re very confident one of those large partners will emerge and take this on,” he says. “It’s just a matter of staying in the race.”


