Fighting the pandemic: Inside the Royal Adelaide Hospital’s intensive care unit
Few in SA have been as intensely affected by coronavirus as the staff in the Royal Adelaide Hospital intensive care unit. This is the inside story of how they’ve held the line against a historic threat.

Coronavirus News
Don't miss out on the headlines from Coronavirus News. Followed categories will be added to My News.
- Social distance warning as shoppers return in droves
- All the latest local, national and global coronavirus coverage
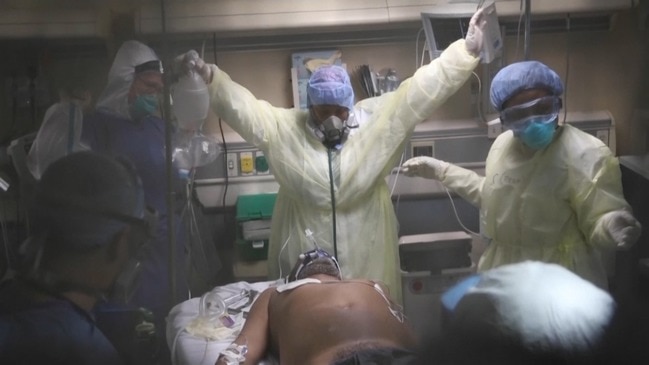
They are the crack team of medicos who have brushed aside their own anxieties and isolation to put themselves in harm’s way to help save the state’s most critically ill coronavirus patients.
Over the past month, in the Royal Adelaide Hospital’s intensive care unit, 110 highly trained doctors, nurses and allied health professionals waged a life-and-death war against a lethal, but invisible, enemy.

At stake were the lives of 18 people, aged between 52 and 77, who all fought for life in isolation, away from their relatives.
While, tragically, four patients lost their brave fight against COVID-19, 14 were discharged under a special guard of honour by a cheering team, who became family in their most desperate hour of need.
The Sunday Mail today reveals the inside story from the state’s COVID-19 epicentre after SA Health granted exclusive access to the elite team of medicos.
In a series of interviews, staff laid bare the fears, challenges and pride at their groundbreaking work that has led to an outpouring of public support.
Some didn’t see their families, or friends, for weeks because they were in self-isolation.
Others came home stressed and emotional. They all, however, were steadfast in their refusal to be transferred from Wing 3.
“They were really protective of the patients, really very much, because their families couldn’t be present,” said the RAH’s acting critical nursing care boss Louise McGuire, 47, a nurse for the past 26 years.
“They felt they were the person who was there for those patients and in place of their family at that time.
“They became extremely protective, which was just really inspiring for me.”
GROUND ZERO

As total local cases hit 197 on March 25, Malcolm Todd, 76, and Paul Faraguna, 68, were admitted to the ICU.
Mr Todd, of Barmera, became the third person to die of the disease in SA on April 8. Mr Faraguna, of Rosslyn Park, was last week discharged to a general ward, where he is recovering.
Dr David Evans, 54, an ICU specialist for 20 years, said patients suffered organ failure and breathing problems, requiring some to be placed into induced comas and on ventilators.
“The feeling when you know they are finally better is a feeling of almost relief because they had been unwell for a long time,” he said.
“They had multiple organ systems that were failing and they were approaching … the limit of what could be done.
“At that point, either they recovered or if they deteriorated further, they passed away.”
Teams of at least 20 staff worked over three shifts – eight hours during the day and 10 hours overnight.
MORE NEWS:
Why politicians are refusing to download the COVID-19 app
Don’t smash Crows players for iso breach: Nicks
Older Australians warned as 5.4 million get app
The work was mentally and physically draining as they were required to wear extensive personal protective equipment, while numbers were restricted bedside.
Even the tea rooms were split to help stop the virus spreading.
“I think it would be fair to say that all of the staff took such pride in wanting to have the privilege in looking after someone in those circumstances,” said ICU specialist of 15 years Dr Stewart Moodie, 48.
“It was difficult, but they absolutely wanted to do it.”
Families were phoned twice daily with updates as medicos constantly grappled with sadness that no relatives could maintain bedside vigils.
Mandy Kocher, 52, an ICU nurse for the past 28 years, whose role was to phone families, said this was especially hard after a death.
“The fact we don’t have a loved one there – that’s really quite a foreign concept in ICU,” she said.
“It is certainly very foreign to all the clinicians. Families are the first, second and third people that should be involved around end of life. I was really quite overwhelmed for their care for us when we were sitting here really worried and caring for them.”
POSITIVE TEST
As the virus spread across the globe, urgent plans were drawn up on how best to treat critically ill patients while protecting staff from the highly contagious disease.
“There was a lot of anxiety until you worked in there because there was that fear of ‘Am I at risk, what are the processes and protocols, how do I care for the patient, their families and myself?’,” Ms McGuire said.
“Once people were in that space, it seemed to allay those fears.”
Amid mounting concerns the system would be “overwhelmed” by an unknown number of cases, a further 259 nurses were trained to work alongside the 505-strong ICU team.
More than a third were moved to other areas for a variety of health reasons. Andrew Barrett, 44, an ICU nurse for 16 years, said: “We just never knew when it was going to come and how big it was going to be.
“I think that was the biggest challenge. We developed a real ‘in the trenches’ type of camaraderie.”
But on April 14, the unit was rocked when a nurse, aged in her 20s, became infected, causing 34 colleagues to be quarantined for a fortnight. How, or where, she caught it remains unknown.
Ms McGuire, who said the nurse recovered at home and had returned to work, paid tribute to nurses who volunteered to cover shifts for isolating colleagues.
“For a lot of us, that was the most stressful week,” she said. “Having to speak with all the staff who already had fears about potential transmission and that then coming to reality.
“It was frightening. The staff involved were extremely distressed. She was more concerned about other people rather than herself. Amazing.
“All the other staff had a mixture of feelings, as you could imagine. Some were like ‘That’s OK it was to be expected,’ whereas other people expressed some fear.”
SUPPORT
There are today no coronavirus patients in the 38-bed unit. While the team is devastated four patients died, they have among the highest survival rates in the country.
Protocols have changed, while technology, such as videoconferencing, allowed families a chance to see their sick relative.
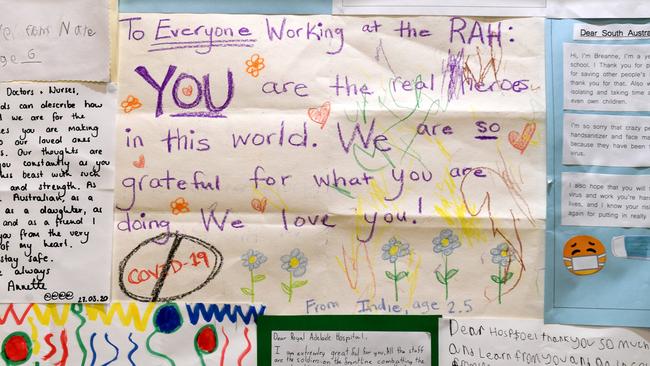

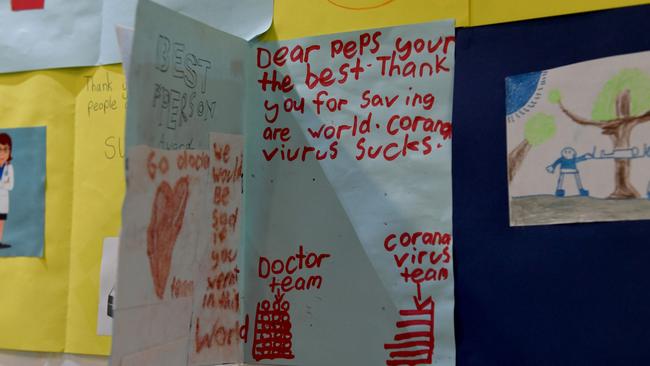
Special photos have been issued to families as “mementos”, while staff maintain contact. Public support is immense, with cards, letters and gifts inundating the hospital.
Mr Barrett said patients were “chuffed” by the guard of honour.
“You develop bonds with them,” he said.
“Some of them didn’t know who we were as they had been asleep for a majority of their journey. We had spent day and night next to them.
“We felt that we knew them, and so when they were leaving, it was amazing to see. It was a massive win.”

Angels fought so hard to save lives
The families of the four Adelaide grandparents who each lost their battles against coronavirus in Royal Adelaide Hospital’s intensive care unit have paid heartfelt tributes to the dedicated team.
The widow of retired Riverland businessman Malcolm “Mal” Todd, 76, of Barmera, praised the compassion shown for him before he died.
Staff had phoned Sandi Todd, 74, twice a day as she was stuck in isolation after the pair contracted the virus during a Barossa Valley visit in late March.
“They didn’t have to arrange a Skype call; they could have just let him pass without me saying goodbye,” she said.
“When we could speak with him, he was in an induced coma but one of the nurses, who was so lovely, was there stroking his arm.
“I was so pleased he had human contact before he died. I can’t thank them enough for what they did.”


The daughter of Ruby Princess cruise ship passenger Linda Lavender, 62, who died on April 8 after spending five days in the ICU, said her family were indebted to the medical staff.
“They were just amazing to her,” said Jaime Day, 31, of Morphett Vale.
“I think of those people often for what they did for her. Their treatment wasn’t just their job – they went above and beyond to make sure she was comfortable.”
The widow of grandfather Roger Leaney, 74, of Valley View, who also contracted the virus on the Ruby Princess, has also thanked doctors.
The retired Australian National Rail diesel fitter, a highly respected community stalwart, died on April 11 after losing his 10-day fight for life.
“Veronica would like to thank the angels in the (RAH) ICU for their compassionate and dedicated care of Roger,” a family statement said.
The family of grandfather Francesco “Frank” Ferraro, 75, of Campbelltown, also thanked staff.
“Despite the best efforts of the medical professionals and staff and the love and support of his family, he passed away,” they said after the retired labourer became the state’s first virus COVID-19 victim on April 6.